General Information about Deltasone
In ulcerative colitis, Deltasone is prescribed to reduce irritation and relieve symptoms such as stomach pain, diarrhea, and rectal bleeding. It works by focusing on the immune system and reducing the manufacturing of chemical compounds that trigger inflammation in the colon.
Deltasone is primarily used to deal with situations that involve irritation, including allergic reactions, bronchial asthma, rheumatoid arthritis, and certain skin problems. It can be helpful in managing situations such as ulcerative colitis, which is a type of inflammatory bowel illness, and multiple sclerosis, which is an autoimmune disorder.
Before starting Deltasone treatment, it's necessary to debate the potential risks and advantages with a healthcare provider, especially if the affected person has a history of allergic reactions or other medical situations.
Like another medicine, Deltasone is associated with some potential side effects. The most common unwanted aspect effects include increased urge for food, weight acquire, temper adjustments, issue sleeping, and an increased threat of infections. These unwanted effects often subside as quickly as the medication is discontinued or the dosage is lowered.
In some instances, Deltasone may also trigger extra extreme unwanted facet effects, including hypertension, diabetes, osteoporosis, and cataracts. It is crucial to inform the physician of any pre-existing medical circumstances before starting Deltasone remedy.
Deltasone is a medication that falls underneath the class of corticosteroids, that are hormones produced by the adrenal glands. It is often prescribed to reduce irritation and alleviate symptoms in varied conditions corresponding to ulcerative colitis and bronchial asthma.
It is essential to notice that Deltasone shouldn't be stopped abruptly, as it could trigger withdrawal symptoms corresponding to fatigue, joint ache, and fever. The dosage ought to be progressively lowered underneath the supervision of a medical skilled to keep away from these signs.
For bronchial asthma patients, Deltasone helps to minimize back airway inflammation and improve respiratory. It does so by decreasing the production of mucus and swelling within the airways, making it simpler for air to flow in and out of the lungs.
One of the main functions of Deltasone is to suppress the immune system's response to irritation, which is the body's pure response to harm or infection. By doing so, it helps to scale back redness, swelling, pain, and other signs associated with irritation.
Deltasone is out there in varied forms, including tablets, liquid, and injectable form. The dosage and duration of remedy rely upon the precise situation being handled, the severity, and the patient's response to the medication.
In conclusion, Deltasone is a extensively used medication for managing various situations that contain irritation. It is a potent anti-inflammatory drug that helps to scale back symptoms and improve the quality of life for sufferers. However, you will want to use this medicine beneath the guidance of a medical skilled and to focus on the potential side effects. With correct use, Deltasone could be an effective and essential treatment option for those affected by inflammatory situations.
While breast cancer and prostate cancer are the most common noncutaneous forms of cancer in men and women best allergy medicine 2014 order deltasone no prescription, respectively, lung cancer is the leading cause of cancer-specific mortality accounting for nearly 30% of cancer deaths in both genders. Disparities in cancer occurrence and mortality persist despite a reduction in the overall age-adjusted mortality from cancer. Cancer incidence remains highest in the United States among white individuals, likely due to their high rates of lung and female breast cancer. However, black men continue to have the highest gender-specific cancer incidence among men and the highest mortality rates despite considerable reductions in cancer mortality for all genders and races. While white women have the highest cancer incidence among women, black women have the highest gender-specific cancer mortality rate despite gradually falling rates for all races. Cancer mortality rates in developed countries are consistently higher among those from racial and ethnic minority groups, especially African Americans, and among those from lower socioeconomic strata. Greater mortality rates among racial and ethnic minorities are not fully explained by differences in the stage at diagnosis. Socioeconomic factors, access to appropriate treatment, and comorbidities represent additional determinants of greater cancer mortality. To facilitate comparisons of rates between populations, rates are often adjusted for age, sex, race, or other demographic characteristics. The association between a characteristic or exposure with cancer risk is generally assessed in either cohort or case-control studies. Cohort studies are generally prospective and evaluate disease experience in exposed and unexposed individuals whereas case-control studies assess the exposure experience in individuals with and without disease. The larger the study population, the more precise the estimate of association is between exposure and disease. However, proper interpretation of the results must explore whether any systematic error or bias has been introduced during the study design or analysis. Confounding factors may obscure or weaken a true association or create a false association because of an association between the factor and both the exposure and disease. Confounding can be evaluated and adjusted for in stratified or multivariate analysis if the potential confounder is recognized and has been properly measured in the data. It is generally not safe to assume that all possible confounding factors have been considered. Therefore, causal inference is seldom justified on the basis of a single study but evolves gradually with study repetition and consideration of other information including animal and other laboratory results, the strength of the association, and a careful consideration of likely confounding factors. Interventions for cancer prevention and screening are generally studied in randomized controlled trials requiring large numbers of participants, close monitoring for adherence in the intervention, long-term follow-up, and appropriate ascertainment of disease and disease-free status. While important for our understanding of carcinogenesis, only a small proportion of cancers are inherited in a mendelian fashion. Neoplasms inherited in an autosomal dominant manner include retinoblastomas, multiple endocrine neoplasia syndromes, and polyposis coli. Several additional pre-neoplastic conditions demonstrate mendelian inheritance with variable penetrance. Several common malignancies demonstrate familial risk patterns with low penetrance, including breast cancer and colorectal cancer. Genetic testing and potential preventative measures are available for several inherited cancer syndromes (Table 55. The proportion of individuals with disease in the population at a given point in time is the prevalence whereas incidence and mortality rates represent the number of events in a population over a defined period of time. Such testing requires a reasonable understanding of cancer genetics as well as the target population along with relevant ethical, economic, and societal issues. At the same time, acquired somatic mutations are universally identified in malignant cells with some clearly driving the development and progression of cancer. While random genetic mutations occur frequently, proto-oncogenes involved in cell growth and proliferation, tumor suppressor genes involved in regulation of cellular proliferation, and mismatch repair genes associated with chromosomal instability play critical roles in carcinogenesis, tumor growth, progression, invasion, and metastasis. Fortunately, the spontaneous mutation rate is relatively low, and more than one mutational event is usually necessary for complete carcinogenic transformation resulting in a malignancy. The vast majority of lung cancers are attributable to cigarette smoking while exposure to secondhand smoke increases the risk for lung cancer in nonsmokers. Cigarette and cigar smoking and chewing tobacco are major risk factors for head, neck, mouth, and esophageal cancers and are associated with development of stomach, pancreas, kidney, bladder, and cervical cancer as well. While tobacco use has declined in the United States over the past two decades, it continues to be unacceptably high, especially among younger women, and continues to increase in many parts of the developing world. Nutrition Diet and body weight appear to play an important role in cancer causation. Excess alcohol use is clearly a significant risk factor for cancers of the liver, head and neck, esophagus, and breast. Obesity and dietary fat intake are associated with colon and breast cancers, but the exact nature of the relationship is still under investigation. Central or visceral adiposity in both men and women is associated with increased incidence and mortality from a number of cancers, including endometrium, breast in postmenopausal women, kidney, gallbladder, pancreas, esophagus, colon, and prostate. Lifestyle Acquired risk factors for cancer include lifestyle factors as well as occupational and other environmental exposure to carcinogenic substances. Major lifestyle risk factors include tobacco, alcohol and other dietary factors, as well as lack of physical activity (Table 55. Tobacco Tobacco products are, by far, the single greatest contributor to cancer incidence and mortality worldwide.
Antibiotics that penetrate pancreatic tissue allergy treatment relief buy 20 mg deltasone with visa, including cephalosporins, carbapenems, quinolones, and metronidazole, are used for treatment of infected necrosis. Risk assessment should be performed for all patients to stratify the severity of illness. Mild acute pancreatitis, the most common form, is characterized by the absence of organ failure and pancreatic necrosis. Mild pancreatitis usually does not require pancreatic imaging, and patients recover within several days with restoration of normal pancreatic function and gland architecture. Patients with mild acute pancreatitis account for 80% of all attacks and less than 5% of the overall mortality rate. Moderately severe pancreatitis is characterized by local complications and/or transient organ failure over a time period of less than 48 hours. Local complications include pancreatic necrosis (with or without infection) and acute peripancreatic fluid collections or pancreatic pseudocysts. Death from moderately severe pancreatitis is much less common than in cases of severe pancreatitis. Severe acute pancreatitis is defined by persistent organ failure extending for more than 48 hours. Most individuals with persistent organ failure have underlying necrotizing disease. Early deaths (within the first week) are most often the result of multiple organ failure caused by the release of inflammatory mediators and cytokines. The risks of infection and death correlate with disease severity and pancreatic necrosis. The overall mortality approaches 30% among patients with persistent organ failure. Despite the importance of recognizing severe disease, most patients are initially admitted to the hospital without necrosis or organ failure, and methods to predict individuals more likely to progress to severe disease during the initial several days of hospitalization have been defined. Regardless of the prognostic factor chosen, there are significant limitations in predicting disease severity. Clinical predictors of a poor outcome include severe comorbid illnesses, older age (60 years), obesity, and long-term, heavy alcohol use. Laboratory findings associated with increased mortality include blood urea nitrogen elevation (>20 mg/dL) on admission or a rise during the first 24 hours of admission, hemoconcentration from third spacing of fluids reflected by an elevated hematocrit of 44 or greater on admission, and serum markers reflecting a robust systemic inflammatory response, such as a C-reactive protein level greater than respiratory, renal, or vascular organ failure. Intra-abdominal hypertension typically occurs early and is the result of pancreatic inflammation and fluid third spacing. Abdominal compartment syndrome is associated with mortality rates ranging up to 50% to 75% in various reports. Suggested treatment includes analgesics, sedation, nasogastric tube decompression, and fluid restriction. If these measures do not result in improvement, percutaneous catheter decompression followed if unsuccessful by a surgical laparotomy is recommended. The ability of this approach to improve outcomes is the focus of ongoing research. Diagnosis and Differential Diagnosis the diagnosis of acute pancreatitis is based on a combination of clinical, biochemical, and radiologic factors. A diagnosis of acute pancreatitis requires two of the following three features: abdominal pain characteristic of acute pancreatitis; serum amylase or lipase levels, or both, at least three times the upper limit of normal; and characteristic findings of acute pancreatitis on imaging. Elevated serum amylase levels may occur in a wide variety of other conditions, including bowel perforation, intestinal obstruction or ischemia, acute appendicitis, cholecystitis, tubo-ovarian disease, and renal failure. Serum amylase levels may be normal in patients with hypertriglyceridemia or alcohol-induced acute pancreatitis. Serum lipase is preferred because it is more sensitive and specific than serum amylase for the diagnosis of acute pancreatitis. The serum lipase level remains normal in some nonpancreatic conditions associated with an elevated serum amylase level, including macroamylasemia. The serum lipase concentration is more sensitive than that of amylase because it remains elevated longer and may be diagnostic even for patients seeking medical attention several days after symptom onset. Repeated measurements of serum pancreatic enzymes have little value in assessing clinical progress, and the magnitude of serum amylase or lipase elevation does not correlate with the severity of pancreatitis. Imaging findings supporting acute pancreatitis include pancreatic enlargement, peripancreatic inflammatory changes, and extrapancreatic fluid collections. Imaging does not exclude the diagnosis of acute pancreatitis because the pancreas appears normal in 15% to 30% of those with mild disease. Pancreatic imaging should be performed after adequate fluid resuscitation to minimize the risk of contrast-induced nephrotoxicity. Early imaging (within 72 hours of symptom onset) can underestimate the existence and extent of pancreatic necrosis. Transabdominal ultrasonography should be performed in all patients with acute pancreatitis when considering a diagnosis of gallstone pancreatitis. Each variable adds 1 point to the total score, and scores of 3, 4, and 5 correspond to mortality rates of 5. Imaging studies predicting a severe outcome include a pleural effusion seen on chest radiography within the first 24 hours or pancreatic imaging identifying necrosis. Severe pancreatitis is predicted by organ dysfunction, including shock (systolic blood pressure <90 mm Hg), respiratory failure (Pao2 60 mm Hg), and acute renal injury (creatinine >2. With increasing scores, the likelihood of a complicated, prolonged, and fatal outcome increases. Analgesia Despite the theoretical concern that narcotic analgesia may result in sphincter of Oddi spasm and worsening pancreatitis, there is no evidence to support withholding narcotics from patients with acute pancreatitis.
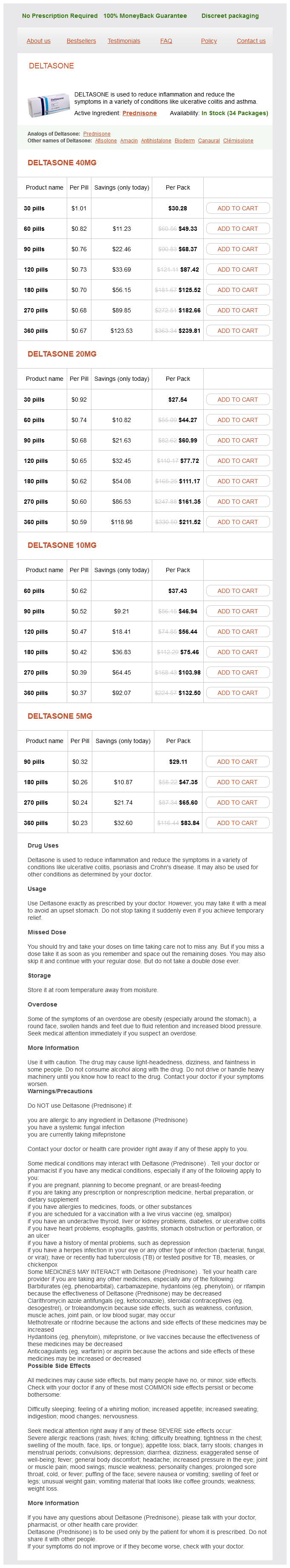
Deltasone Dosage and Price
Deltasone 40mg
- 30 pills - $30.28
- 60 pills - $49.33
- 90 pills - $68.37
- 120 pills - $87.42
- 180 pills - $125.52
- 270 pills - $182.66
- 360 pills - $239.81
Deltasone 20mg
- 30 pills - $27.54
- 60 pills - $44.27
- 90 pills - $60.99
- 120 pills - $77.72
- 180 pills - $111.17
- 270 pills - $161.35
- 360 pills - $211.52
Deltasone 10mg
- 60 pills - $37.43
- 90 pills - $46.94
- 120 pills - $56.44
- 180 pills - $75.46
- 270 pills - $103.98
- 360 pills - $132.50
Deltasone 5mg
- 90 pills - $29.11
- 180 pills - $47.35
- 270 pills - $65.60
- 360 pills - $83.84
Treatment with formulas rich in branched-chain amino acids has shown no benefit in improving encephalopathy or mortality allergy symptoms night generic deltasone 40 mg without a prescription. Contributors include the inadequate hepatic removal of potential endogenous neurotoxins, altered permeability of the blood-brain barrier, and abnormal neurotransmission. It is characterized by gas exchange abnormalities (increased alveolar-arterial gradient and hypoxemia) resulting from intrapulmonary vascular dilation. The vascular dilation leads to vascular remodeling and angiogenesis, resulting in impaired oxygen transfer from the alveoli to the central stream of red blood cells within capillaries. Usually, this functional intrapulmonary right-to-left shunt significantly improves with the administration of 100% oxygen. Intrapulmonary shunting is demonstrated by contrast echocardiography, in which agitated saline is injected into a peripheral vein during the performance of two-dimensional echocardiography. Delayed appearance of microbubbles in the left cardiac chambers (more than three to six cardiac cycles after injection) indicates intrapulmonary vasodilation. Early visualization of microbubbles in the left cardiac chambers indicates intracardiac shunting. Other tests, including chest radiography, computed tomography, and pulmonary function tests, are performed to exclude intrinsic cardiopulmonary disorders. Patients are usually directed to achieve two to three soft stools per day as the goal of lactulose therapy. Reduction and elimination of nitrogenous compound substrates can also be achieved by administering enemas and using nonabsorbable antibiotics such as rifaximin in patients who do not tolerate or respond to lactulose. Other agents that affect intestinal motility and ammonia generation are being evaluated, including acarbose and probiotics. Clinical Presentation Clinical features range from subclinical abnormalities in gas exchange to profound hypoxemia causing significant dyspnea. Screening and Treatment Screening by pulse oximetry typically targets patients with values lower than 96% at rest on room air for further evaluation; however, recent data suggest that this may not be an appropriate screening tool. Recent evaluation of newer agents such as sorafenib showed no significant improvement. The exact pathophysiologic mechanisms leading to tumor genesis in patients with other causes of cirrhosis. The diagnostic values include a mean pulmonary arterial pressure greater than 25 mm Hg at rest or 30 mm Hg with exercise, a pulmonary capillary wedge pressure lower than 15 mm Hg, and a pulmonary vascular resistance greater than 240 dynes, all in the presence of portal hypertension or liver disease or both. Histologically, it has characteristics similar to those of pulmonary hypertension. A tissue specimen may be necessary to confirm the diagnosis in some cases, but it is not needed if characteristic clinical and radiologic features are present, especially if they are accompanied by a rise in serum -fetoprotein levels. Treatment Patients with well-compensated cirrhosis may undergo surgical resection or liver transplantation, with a 5-year survival rate of up to 70%. However, recently another agent was approved, lenvatinib, which works by the same mechanism, and both have been shown to prolong survival of these patients. Second-line agents have also been approved, which include regorafenib, cabozantinib, and nivolumab. Prognosis In patients with widespread, multifocal disease and in those with vascular invasion, the prognosis is poor, with a 5-year survival rate of 5% to 6%. Accordingly, emphasis is placed on prevention of viral hepatitis and other causes of liver disease and on screening by ultrasound of those who are at higher risk, including patients with known cirrhosis. One study observed that as many as 25% to 65% of patients with splanchnic vein thrombosis in the absence of cirrhosis had a myeloproliferative disease. The disease produces the manifestations of portal hypertension, but the liver histology is usually normal. Diagnosis the diagnosis is established by angiography, but noninvasive imaging modalities such as Doppler ultrasonography, computed tomography, and magnetic resonance imaging may reveal thrombus, collateral circulation near the porta hepatis, and splenomegaly. In most patients, recanalization of the thrombus occurs within 6 months after initiation of anticoagulation. Recommendations for duration of anticoagulation after an acute event vary and are usually 3 to 6 months. Long-term anticoagulation may be used in cases of chronic thrombosis, especially when associated with hypercoagulable states. Prophylaxis with -blockers to prevent variceal bleeding may decrease the portal pressure, potentially propagating thrombus, and therefore is not usually recommended. If endoscopic treatment fails, surgical management with portosystemic shunting may be attempted, but this approach is often difficult because of the absence of suitable patent vessels. Abdominal trauma and congenital webs of the vena cava are also related to Budd-Chiari syndrome. About 20% of cases are idiopathic, but many of these patients prove to have early, subclinical myeloproliferative disease or genetic mutations associated with a hypercoagulable state. Affected patients usually have portal hypertension with or without associated liver dysfunction, which may mimic the presentation of cirrhosis. Portal Vein Thrombosis Definition and Etiology Thrombosis of the portal vein may develop after blunt abdominal trauma, umbilical vein infection, neonatal sepsis, intra-abdominal inflammatory diseases. Myeloproliferative diseases Clinical Presentation Budd-Chiari syndrome can manifest acutely, possibly in association with acute liver failure, or it can manifest as a subacute or chronic illness. Acute disease produces right upper quadrant abdominal pain, hepatomegaly, ascites, and jaundice, whereas the subacute or chronic form produces primarily portal hypertension.
© 2025 Adrive Pharma, All Rights Reserved..