General Information about Cytoxan
Cytoxan, also referred to as cyclophosphamide, is a chemotherapy drug primarily used to deal with varied kinds of most cancers. It is a powerful treatment that works by slowing or stopping the growth of cancer cells within the physique. Let's take a extra in-depth look at what Cytoxan is, how it works, and what forms of most cancers it's used to deal with.
Blood and lymph system cancers like leukemia and lymphoma are often treated with Cytoxan together with other chemotherapy medication and radiation remedy. In kids with neuroblastoma or Wilms tumor, that are uncommon forms of nerve and kidney cancers respectively, Cytoxan is used as part of the initial therapy together with other medications.
In ovarian most cancers, Cytoxan is commonly utilized in mixture with other chemotherapy medication after surgery to kill any remaining cancer cells and stop the most cancers from recurring. In breast cancer, it could be given earlier than or after surgical procedure and can also be used to treat metastatic breast most cancers that has spread to other elements of the body.
How does it work?
Cytoxan, also recognized by its generic name cyclophosphamide, is a sort of alkylating agent. Alkylating brokers are chemotherapy medication that work by damaging the DNA of cancer cells, inflicting them to die. Cytoxan is available in both oral and injectable forms and is often prescribed in combination with different chemotherapy medication to deal with varied forms of most cancers.
Possible unwanted side effects
Other much less common however more critical unwanted effects may embody bladder damage, which can result in bleeding or issue urinating, and an increased risk of growing different kinds of cancer. Your doctor will monitor you closely throughout therapy to check for these unwanted facet effects and regulate your dosage if needed.
Like all chemotherapy drugs, Cytoxan might cause some unwanted facet effects. The most common unwanted effects include nausea, vomiting, hair loss, diarrhea, and bone marrow suppression, which might increase the chance of infection, anemia, and bleeding. However, these unwanted aspect effects may be managed with different medications and usually improve as soon as treatment is completed.
What is Cytoxan?
What kinds of cancer is it used to treat?
Cytoxan is used to treat a variety of cancers, together with ovarian most cancers, breast cancer, blood and lymph system cancers like leukemia and lymphoma, retinoblastoma (a cancer of the eye discovered primarily in children), multiple myeloma (a cancer of the bone marrow), and mycosis fungoides (a type of pores and skin cancer).
In conclusion, Cytoxan is a crucial chemotherapy drug that is used to treat a range of cancers. It works by damaging the DNA of most cancers cells, making it an efficient therapy possibility for lots of forms of cancer. Although it could cause some unwanted effects, these may be managed with proper medical care. If you or a loved one is receiving Cytoxan as part of your cancer remedy, it is essential to follow your doctor's instructions and attend all scheduled appointments to ensure the very best consequence.
Cytoxan works by interfering with the growth and division of most cancers cells. It does this by attacking the DNA of cancer cells, preventing them from reproducing and spreading. Unlike different chemotherapy drugs that target quickly dividing cells, Cytoxan is active in all phases of the cell cycle, making it efficient in treating a variety of cancers.
Cytoxan can also be used to deal with multiple myeloma, a cancer that starts within the bone marrow, by killing the most cancers cells and slowing the progression of the disease. And in mycosis fungoides, a type of skin most cancers, Cytoxan is used to shrink tumors and relieve signs.
The encephalitic form presents with the hydrophobia treatment walking pneumonia 50 mg cytoxan order with mastercard, delirium, and agitation that form the common picture of rabies. About a fifth of patients present with the paralytic form and have little clinical evidence of cerebral involvement until late in the course. The spinal cord and brainstem bear the brunt of the illness in the paralytic form. The pathogenetic distinction between the two types of rabies is unclear; it does not appear to be based on virologic or antigenic differences. Sir William Gowers112 provides a seminal depiction of hydrophobia and its sequelae, in which he described: ". As the intensity of the spasm increases, so does the readiness with which it is excited. It may be caused by the mere contact of water with the lips, and a state of cutaneous hyperæsthesia develops, so that various impressions, such as a draught of air, which normally excite a respiratory effort, bring on the spasm. The patient is often unable to swallow the saliva, which is usually abundant and viscid, so that it hangs about the mouth and is expelled with difficulty. The attacks of spasm are very distressing to the patient; the mental state which they occasion increases the readiness with which they are produced; and in some cases the mere sight of water or the sound of dropping water will cause an attack. It may even be excited by visual impressions which cause a similar sensation, as the reflection from a looking glass, or even a strong light. The spasm, at first confined to the muscles of deglutition and respiration, spreads to the other muscles of the body, and the paroxysms, at first respiratory, afterwards become general, and assume a convulsive character, although still excited by the same causes. The convulsions may consist of general muscular rigidity, sometimes tetanoid in character, with actual opisthotonus. The mental derangement is most intense during the paroxysms of spasms, and the frenzied patient may spit his saliva at those about him, and often attempts to bite them with his teeth, making occasional strange sounds in his throat which have been thought to resemble the barking of a dog. Patients with encephalitic rabies who receive maximal intensive care support may survive for a longer-than-expected period and appear to pass through the paralytic phase before death. Their initial findings suggest an ascending paralysis, including hypophonia, resembling acute inflammatory polyneuropathy (Guillain-Barré syndrome), or a symmetrical quadriparesis. Meningeal signs (headache, neck stiffness) may be prominent despite a normal sensorium. As the disease progresses the patient becomes confused and then declines into coma. In addition to the cardiac arrhythmias already mentioned, the systemic complications of rabies are similar to those of other critically ill patients. The virus disseminates to many organs,119,120 but proof of its role in other organ dysfunction is lacking. The presentation in areas where domestic animals are immunized is seldom this straightforward. When symptoms begin, standard laboratory testing does not reliably distinguish rabies from other encephalitides. Along with coma, evidence of pituitary dysfunction often develops, especially disordered water balance (either inappropriate antidiuresis or diabetes insipidus). Hyperventilation gives way to forms of periodic and ataxic respiration,113 and eventually apnea supervenes. Cardiac arrhythmias are common, predominantly supraventricular tachycardias, and bradycardias, and they reflect either brainstem dysfunction or myocarditis. During the first week of symptoms, about 50% of samples reveal rabies virus, with an increasing percentage thereafter. In the United States the state health department should be consulted whenever the diagnosis of rabies is suspected. Late in the course, gadolinium enhancement may occur in the most profoundly involved areas, indicating breakdown of the blood-brain barrier. With encephalitic rabies, the major differential consideration is another viral encephalitis. Tetanus is occasionally confused with rabies because opisthotonic posturing may be seen in either. Rabies may be misdiagnosed as cerebral malaria and vice versa: At least one atypical case of the latter presented with phobic spasms. Paralytic rabies may resemble acute inflammatory polyneuropathy, transverse myelitis, or poliomyelitis. Electromyographic studies may be useful in distinguishing rabies from polyneuropathy. In transverse myelitis a finding of pain at the level of the lesion may be helpful, as may the finding of a high T2 signal lesion. A sensory level is characteristic of transverse myelitis, whereas in rabies, sensory function is typically normal. Spongiform changes in brain tissue in rabies143 may resemble those seen in the prion diseases. It resembles encephalitis, or occasionally it presents as a mass lesion that resembles a brain abscess. It typically begins 10 to 14 days after vaccine exposure, which would constitute an unusually brief incubation period for rabies. Prompt consultation with public health officials is advised because this decision is based in part on the current prevalence of rabies in the animal species involved in the exposure. In a recent 17-year population survey of 14,453 households with bedroom bat exposure without a recognized bite, the number of individuals needed to be treated to prevent a single case of bat rabies ranged from 314,000 to 2. Chapter 163 Rabies (Rhabdoviruses) Although management of animal rabies is central to prevention of human disease, very few nations have truly eliminated it, and those that have been successful, in lieu of enzootic wildlife rabies, usually maintain quarantine procedures lest the disease reappear. Prophylaxis for cats and dogs in many countries is required by law; in the United States the use of 1-year or 3-year vaccines is common, although only the 3-year vaccines are recommended.
Dysregulation of cytokines in acute Q fever: role of interleukin-10 and tumor necrosis factor in chronic evolution of Q fever symptoms xxy purchase cytoxan 50 mg. The spread of Q fever from animals to man; the natural history of a rickettsial disease. Histopathology in man and rhesus monkeys in the pneumonitis due to the virus of "Q fever". Prolonged Q fever associated with inappropriate secretion of anti-diuretic hormone. A microagglutination technique for detection and measurement of rickettsial antibodies. The persistence of complementfixing antibodies to Q-fever (Coxiella burnetii) after infection. Detection and persistence of specific IgM antibody to Coxiella burnetii by enzyme-linked immunosorbent assay: a comparison with immunofluorescence and complement fixation tests. Evaluation of the complement fixation and indirect immunofluorescence tests in the early diagnosis of primary Q fever. Antibody responses in acute and chronic Q fever and in subjects vaccinated against Q fever. Q Fever pneumonia: are clarithromycin and moxifloxacin alternative treatments only Antibiotic therapy for acute Q fever in the Netherlands in 2007 and 2008 and its relation to hospitalization. Evolution from acute Q fever to endocarditis is associated with underlying valvulopathy and age and can be prevented by prolonged antibiotic treatment. Treatment and prophylactic strategy for Coxiella burnetii infection of aneurysms and vascular grafts: a retrospective Cohort Study. Q fever in patients with hepatitis and pneumonia: results of laboratory-based surveillance in the United States. Chronic Q fever in the Netherlands 5 years after the start of the Q fever epidemic: results from the Dutch chronic Q fever database. Serological evaluation of O fever in humans: enhanced phase I titers of immunoglobulins G and A are diagnostic for Q fever endocarditis. Phagolysosomal alkalinization and the bactericidal effect of antibiotics: the Coxiella burnetii paradigm. Comparison of different antibiotic regimens for therapy of 32 cases of Q fever endocarditis. Correlation between serum doxycycline concentrations and serologic evolution in patients with Coxiella burnetii endocarditis. Therapeutic impact of the correlation of doxycycline serum concentrations and the decline of phase I antibodies in Q fever endocarditis. Coxiella burnetii infection of aortic aneurysms or vascular grafts: report of 30 new cases and evaluation of outcome. Production of interleukin-10 and transforming growth factor beta by peripheral blood mononuclear cells in Q fever endocarditis. Neurological involvement in acute Q fever: a report of 29 cases and review of the literature. Demyelinating polyradiculoneuritis following Coxiella burnetti infection (Q fever). Severe combined immunodeficiency syndrome, tissue transplant, leukaemia, and Q fever. Chronic or fatal Q-fever infection: a review of 16 patients seen in North-East Scotland (1967-80). Coxiella burnetii, the agent of Q fever, replicates within trophoblasts and induces a unique transcriptional response. Coxiella burnetii seropositivity in parturient women is associated with adverse pregnancy outcomes. Persistence of impaired health status of Q fever patients 4 years after the first Dutch outbreak. Treatment of chronic fatigue syndrome with antibiotics: pilot study assessing the involvement of Coxiella burnetii infection. Improvement of chronic nonspecific symptoms by long-term minocycline treatment in Japanese patients with Coxiella burnetii infection considered to have post-Q fever fatigue syndrome. Effectiveness of long-term doxycycline treatment and cognitivebehavioral therapy on fatigue severity in patients with Q fever fatigue syndrome (Qure Study): a randomized controlled trial. The effectiveness of Coxiella burnetii vaccines in occupationally exposed populations: a systematic review and meta-analysis. Infection control practices and zoonotic disease risks among veterinarians in the United States. Chapter 188 Coxiella burnetii (Q Fever) 189 Rickettsia prowazekii (Epidemic or Louse-Borne Typhus) Lucas S. Brill-Zinsser disease is recurrence of typhus, often in milder form, even decades after the initial infection. A fourfold rise in immunoglobulin G (IgG) titer from acute illness to convalescence confirms the diagnosis. Diagnosis Epidemiology · the agent is transmitted between patients by the human body louse (Pediculus humanus corporis). The organism is inoculated into a new host by scratching of rickettsiae-laden louse feces into louse-bitten skin or by being rubbed into mucous membranes. Treatment and Prevention · Doxycycline, 100 mg twice daily for 7 days, is the treatment of choice. Rickettsia prowazekii is the only rickettsial species that can cause devastating, naturally occurring epidemics capable of killing a substantial proportion of human populations infested with body lice.
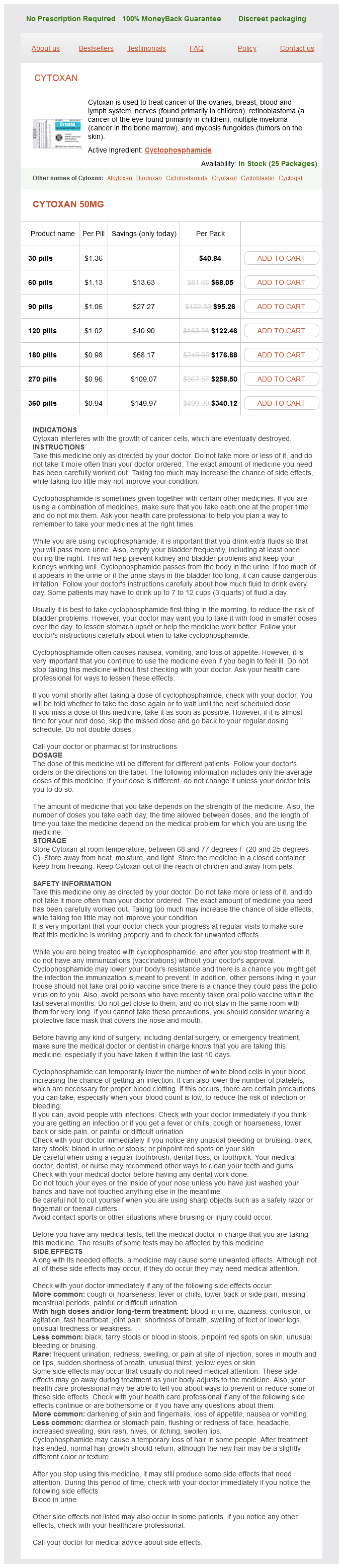
Cytoxan Dosage and Price
Cytoxan 50mg
- 30 pills - $40.84
- 60 pills - $68.05
- 90 pills - $95.26
- 120 pills - $122.46
- 180 pills - $176.88
- 270 pills - $258.50
- 360 pills - $340.12
In a case series that included 92 patients from four of the outbreaks in Bangladesh treatment quincke edema discount 50 mg cytoxan with visa, the case-fatality rate was 74% compared with 38% in the outbreak in Malaysia and Singapore. Given the epidemiologic and clinical differences between Hendra virus and the outbreak of encephalitis in Malaysia, it was proposed that a paramyxovirus that was related to but distinct from Hendra virus had caused the outbreak. Island flying foxes (Pteropus hypomelanus) and Malayan flying foxes (Pteropus vampyrus) were found to have neutralizing antibodies to Nipah virus. Chapter 161 Zoonotic Paramyxoviruses: Nipah, Hendra, and Menangle Viruses Reservoirs and Intermediate Hosts 2120 Other animals may serve as reservoirs of related paramyxoviruses. In 2012, three people who had been working in an abandoned mine in China developed severe pneumonia of unknown etiology and died. The positive anal swab samples were cultured in various cell lines for virus isolation, but no cytopathic effect or viral replication was detected. The only animals that are known to have served as intermediate hosts of Nipah virus are pigs during the initial outbreak in Malaysia and Singapore6,7 and horses during the outbreak of Nipah virus or a related virus in the Philippines. Four patients had leptomeningeal enhancement, and four had enhancement of the parenchymal lesions. In a follow-up study 1 month after the outbreak in Malaysia, 5 of 12 patients had widespread small foci of high signal intensity on the T1-weighted images, especially in the cerebral cortex. At the 6-month follow-up, there was no radiographic evidence of progression or relapse. Four patients had late-onset neurologic abnormalities months after the acute illness. Leukopenia (11%), thrombocytopenia (30%), and elevated levels of alanine aminotransferase (33%) and aspartate aminotransferase (42%) were the most common laboratory abnormalities in the outbreak in Malaysia. Nipah virus causes a multiorgan vasculitis with a predilection for the central nervous system. This was most marked in the central nervous system, although the lungs, heart, and kidneys were also involved. Immunohistochemistry revealed the presence of Nipah virus antigens in the endothelial and smooth muscle cells of blood vessels, and in neurons and other affected cells. In experimental infections in African green monkeys, a Nipah virus strain from Bangladesh was uniformly fatal, whereas a strain from Malaysia was fatal in only half of infected monkeys. The mainstay of therapy for Nipah virus infection is supportive care, including monitoring in the intensive care unit for patients with severe illness. In an open-label study of oral or intravenous ribavirin in patients with Nipah virus encephalitis in Malaysia, 45 of 140 patients (32%) in the ribavirin group died, compared with 29 of 54 (54%) in the control group. On the basis of its in vitro activity against Nipah virus, the antimalarial agent chloroquine was assessed, individually and in combination with ribavirin, for the treatment of Nipah virus infection in a golden hamster model. Chloroquine did not protect hamsters when administered either alone or in combination with ribavirin. In another study, ribavirin delayed but did not prevent death in hamsters after a lethal challenge with Nipah virus. It has been suggested that diverting a larger proportion of the supply of date palm sap to be used for making molasses will help reduce Nipah virus infections because the sap is heated to temperatures at which Nipah virus cannot survive during the manufacturing process. Chapter 161 Zoonotic Paramyxoviruses: Nipah, Hendra, and Menangle Viruses Laboratory Abnormalities Prevention Diagnostic Tests Pathology Therapy In September 1994, an outbreak of an acute respiratory illness occurred in thoroughbred horses in Hendra, a suburb of Brisbane in Queensland, Australia. During the next 2 weeks, 13 more horses at the same stable died or were euthanized. Three more horses were found to have seroconverted without having had signs of clinical illness. Within 1 week of the death of the equine index case, a horse trainer and a stablehand became ill with a severe influenza-like illness. The trainer died after developing respiratory and renal failure, whereas the stablehand recovered. The first horse was a pregnant thoroughbred that had developed severe respiratory distress, ataxia, and swelling of the cheeks and supraorbital fossa during a 24-hour period. The second horse, a 2-year-old colt, died 11 days later, after a 24-hour clinical course of aimless pacing, muscle trembling, and hemorrhagic nasal discharge. The etiologic agent was originally called equine morbillivirus, but the name was later changed to Hendra virus, after the suburb where the first outbreak had been identified. An outbreak in five horses in Brisbane, Queensland, in July 2008 resulted in Hendra virus infection in two veterinary workers, one of whom died. In addition to Queensland, several cases have occurred in horses in New South Wales. A serologic survey of wildlife species that were present at the site of the outbreaks was performed. Nomadic birds and flying foxes (bats of the Pteropus genus) were then targeted as likely reservoirs, given their presence in the regions of both outbreaks and their ability to travel long distances. AntiHendra virus antibodies were found in several types of flying fox throughout Queensland. Hendra virus was subsequently isolated from the reproductive tract of a pregnant gray-headed flying fox that had become entangled on a wire fence and from tissue from aborted flying fox fetuses. Urine was the most common specimen type to be positive (26 of 29 urine specimens). Another individual had a dry cough, sore throat, cervical lymphadenopathy, myalgias, fatigue, and fever that lasted for 4 days. Another patient presented with a similar syndrome but rapidly developed respiratory distress necessitating mechanical ventilation. Two patients presented with an influenza-like illness, with subsequent progression to encephalitis; one of these patients recovered and the other one died. Relapsed disease manifesting as encephalitis occurred in one patient 14 months after a horse that he had cared for died from Hendra virus.
© 2025 Adrive Pharma, All Rights Reserved..