General Information about Cystone
In addition to its advantages for the urinary tract, Cystone additionally has a diuretic effect. It helps improve the quantity and frequency of urination, which is important for flushing out toxins and preventing the buildup of dangerous bacteria. The elevated urinary circulate also helps prevent the formation of crystals and stones by diluting the urine and increasing its pH degree.
Another crucial facet of urinary tract well being is sustaining the integrity of the mucosal lining of the urinary tract. The mucosal lining helps shield the urinary tract from the harmful effects of micro organism and toxins. When this barrier is compromised, it can result in inflammation and infection. Cystone incorporates anti-inflammatory and antispasmodic properties that assist soothe and protect the mucosal lining, promoting its pure therapeutic process.
Furthermore, Cystone additionally supports regular urine composition. It helps prevent the formation of crystals and stones in the urinary tract. This is especially helpful for people who discover themselves prone to kidney stones. The potent components in Cystone inhibit the growth and accumulation of minerals in the urinary tract, thus lowering the danger of stone formation. Additionally, it also helps dissolve small stones, making them simpler to move naturally.
One of the key advantages of Cystone is its capacity to forestall and treat urinary tract infections. UTIs are caused by the overgrowth of bacteria within the urinary tract, leading to inflammation and infection. Cystone incorporates anti-microbial properties that help combat the harmful micro organism and forestall their adherence to the walls of the urinary tract. This, in flip, helps prevent the unfold of infection and promotes the therapeutic of infected tissues.
Cystone is a natural supplement that has been used for centuries in Ayurvedic medicine to promote urinary tract health. It is a proprietary blend of highly effective components, together with Shilapushpa (Didymocarpus pedicellata), Pasanabheda (Saxifraga ligulata), and Manjishtha (Rubia cordifolia), amongst others. These natural ingredients work collectively to support the traditional functioning of the urinary tract by sustaining proper urine composition and mucosal integrity.
In conclusion, Cystone is a pure, protected, and efficient approach to promote a wholesome urinary tract. Its potent ingredients work synergistically to prevent and treat UTIs, promote normal urine composition, and keep mucosal integrity. Moreover, it is free from any adverse unwanted effects and can be safely used as a long-term solution to maintain urinary tract concord. So, for anyone trying to naturally help their urinary tract well being, Cystone is certainly a complement to assume about.
Urinary tract well being is an important aspect of total well-being. It performs a vital role in eliminating waste products and toxins from the physique and maintaining a balanced pH degree. However, varied factors corresponding to dehydration, poor diet, insufficient hygiene, and bacterial infections can disrupt the conventional functioning of the urinary tract. This can lead to a host of uncomfortable and often painful conditions, including urinary tract infection (UTI) and kidney stones. Fortunately, nature has provided us with a powerful herbal treatment that can help keep a wholesome urinary tract � Cystone.
Cystone has been extensively researched, and its effectiveness has been supported by scientific studies. One examine revealed in the Journal of Clinical and Diagnostic Research confirmed that Cystone has significant antibacterial and anti-inflammatory activity, making it an effective natural remedy for UTIs. Another research published within the International Journal of Advanced Ayurveda, Yoga, Unani, Siddha, and Homeopathy demonstrated the antiurolithiatic (kidney stone preventing) results of Cystone in decreasing stone formation.
This dissection should begin at the bladder neck symptoms jaundice purchase cystone in india, where this fascia forms a thick band. This maneuver releases the bundle laterally, thus making it easier to perform the next step, in which the bundle is released posteriorly at the apex. The lateral surface of the prostate is exposed by displacing the prostate on its side with use of a Babcock clamp. Beginning on the rectal surface, the bundle is released from the prostate by spreading a right-angled clamp gently. Once the dissection has been initiated at the apex, it should proceed to the midpoint of the prostate. Because the superficial layers of the levator fascia have already been released, this dissection often proceeds easily. Furthermore, in using this plane, the Denonvilliers fascia and prostatic fascia remain on the prostate; only the residual fragments of the levator fascia are released from the prostate laterally. At this point in the procedure, the bundle should be released to the seminal vesicle. Usually it is not necessary to clip the prostatic side of these tiny vessels; fine scissors should be used to divide them. The surgeon should be aware that the bundle may travel more anteriorly in some patients. The apical approach to the bundle facilitates management of this condition as well. Using the principles described previously, positive surgical margins in patients with organ-confined disease that are caused by inadvertently cutting into the prostate are rare. The purpose of this approach is to speed up the recovery of sexual function and continence by reducing traction on the branches of the nerves to the cavernous bodies and striated sphincter or to avoid inadvertent transection of the small branches that travel anteriorly (Costello et al, 2004; Takenaka et al, 2004, 2005; Horninger et al, 2005; Menon et al, 2005; Montorsi et al, 2005). However, because there is less soft tissue at the apex, the risk for positive surgical margins could be increased by this approach. The procedure begins after ligation of the dorsal venous complex and before incision of the urethra. Once total hemostasis is obtained, the levator fascia over the anterior apex of the prostate is incised and the incision is extended distally along the lateral edge of the apex of the prostate, preserving the underlying prostatic fascia. The prostatic fascia is the glistening white fascia immediately below the veins that travel along the lateral surface of the prostate. To identify the correct plane and avoid inadvertent incision into the prostate, it is essential to have excellent visualization and magnification. As the dissection proceeds distally, the levator fascia should be released from the lateral shoulders of the prostate, with care taken not to enter the underlying prostatic fascia. Because the recovery of sexual function at 12 months after unilateral high release was the same as with bilateral high release, we now routinely perform it on only one side, the side with the most favorable pathologic status. If high release of the levator fascia was performed only unilaterally, a rightangled clamp is inserted under the levator fascia at the apex on the side contralateral to the high release. This facilitates identification of the same dissection plane beneath the levator fascia as the contralateral side without the need for approaching the plane by first dividing the levator fascia from the outside. This avoids traction injury, which can occur during wide excision of the contralateral bundle. The bundle is divided without ligation in an effort to excise as much soft tissue as possible. However, to improve exposure, the sponge stick should never be placed on the prostate itself because it may displace tissue, producing a false-positive margin. In developing this plane, all layers of Denonvilliers fascia should be left covering the seminal vesicles. The lateral pedicles are thick, and therefore they need to be divided in a sequential way: superficial, middle, deep (next to the seminal vesicles). If one tries to divide them all at once, this risks cutting into the overlying prostate. The dissection proceeds superiorly onto the anterolateral surface of the junction between the bladder and the prostate. Finally, Denonvilliers fascia is divided over the tips of seminal vesicles to facilitate removal. At this point, many surgeons elect to divide the vasa deferentia and free up the seminal vesicles. The incision is carried down to the mucosa, the mucosa is incised, the Foley balloon is deflated, and the two ends of the catheter are clamped together to provide traction. After these pedicles are divided, it should be possible to visualize the plane between the anterior surface of the seminal vesicles and the posterior wall of the bladder. By scissor dissection hugging the anterior surface of the seminal vesicles, the posterior bladder neck can be divided safely while observing the location of the ureteric orifices. After the posterior bladder wall is divided, the bladder neck is retracted with an Allis clamp, and the vasa deferentia are ligated with hemoclips and divided. Recall that the pelvic plexus is located on the lateral surface of the seminal vesicles. To avoid injury to the pelvic plexus, the surgeon should perform this dissection with great care, especially laterally, and under direct vision should identify the small arterial branches that travel to the seminal vesicles and stay close to the seminal vesicles when these small vessels are ligated with small clips. As the tips of the seminal vesicles are freed, small arterial branches at the tip of each seminal vesicle should be identified, ligated, and divided.
Prostate rebiopsy is a poor surrogate of treatment efficacy in localized prostate cancer symptoms 1 week after conception order discount cystone. Fifteen-year biochemical relapse-free survival, cause-specific survival, and overall survival following I(125) prostate brachytherapy in clinically localized prostate cancer: Seattle experience. Natural history of clinically staged low- and intermediate-risk prostate cancer treated with monotherapeutic permanent interstitial brachytherapy. Treatment planning issues related to prostate movement in response to differential filling of the rectum and bladder. Identification of patients at increased risk for prolonged urinary retention following radioactive seed implantation of the prostate. Posttreatment prostatic-specific antigen doubling time as a surrogate endpoint for prostate cancer-specific survival: an analysis of Radiation Therapy Oncology Group Protocol 92-02. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensitymodulated radiotherapy for localized prostate cancer. Postradiotherapy 2-year prostate-specific antigen nadir as a predictor of long-term prostate cancer mortality. Induced sensitization of tumor stroma leads to eradication of established cancer by T cells. Randomized trial comparing conventionaldose with high-dose conformal radiation therapy in early-stage adenocarcinoma of the prostate: long-term results from Proton Radiation Oncology Group/American College of Radiology 95-09. Radical radiation therapy in the management of prostatic adenocarcinoma: the initial prostate specific antigen value as a predictor of treatment outcome. There is a clear requirement to improve the current therapeutic ratio with novel interventions. Minimally invasive focal therapies in localized prostate cancer offer the potential to reduce side effects and the health care burden and costs associated with radical modalities such as surgery or radiotherapy. This chapter reviews the role of these approaches and the therapeutic dilemma that men with localized low-volume prostate cancer currently face, in the context of novel therapies that aim to find a middle ground-tissue-preserving focal therapy-that follows the paradigm of almost all other solid-organ cancers. Currently, the options often straddle two ends of a spectrum with active surveillance at one end and radical therapy, such as prostatectomy or radiotherapy, at the other. However, although there is a small survival advantage for these men, it could be argued that the morbidity from treatment (urinary incontinence, sexual dysfunction, rectal problems) questions the wholesale application of radical therapy to all men with intermediate- and high-risk disease. The effect was predominantly nested in a minority of countries, suggesting heterogeneity of study conduct, delivery, health care systems, and possibly disease types based on ethnic grounds. Although arguments rage about the strengths and weaknesses of each study, what is very clear is that any advantage from screening and treatment is likely to be small if all cancers are treated uniformly. We are therefore left with a stark choice: either to abandon the screening and diagnosis of prostate cancer as recommended by many high-level health care bodies that provide guidance to governmental institutions, or to find ways to identify men who are likely to benefit from treatment, and to these men offer therapies that reduce the impact on genitourinary and rectal function if they are suitable. Tissue-preserving strategies aim to target the cancer and not the whole organ when it is morphometrically possible to do so and thus reduce damage to collateral tissues. The ultrasound examination is used to identify the prostate itself and not the suspicious lesion; this results in 10 to 12 biopsy specimens being taken blindly throughout the prostate. They have an estimated false-negative rate of 30% to 45% (Djavan et al, 2001; Scattoni et al, 2007). The clinician takes 10 to 12 biopsy specimens in a manner that attempts to obtain representative tissue from the peripheral zone. However, this systematic error leads to several parts of the prostate not being well sampled. First, the anterior part of the gland is missed as a result of its greater distance from the rectum. Second, areas in the midline are undersampled owing to efforts to avoid the urethra. Third, the prostate apex is often inaccessible by the transrectal route (Crawford et al, 2005; Onik et al, 2009; Barzell et al, 2012; Lecornet et al, 2012). As a result of the poor risk attribution, many men and their physicians choose radical therapies from which they derive little to no survival benefit. It is associated with a number of complications, the most important being urinary tract infection (1% to 8%) that can result in life-threatening sepsis (1% to 4%). Hematuria (50%), hematospermia (30%), pain or discomfort (most), dysuria (most), and urinary retention (1%) can also be expected (Abdelkhalek et al, 2012; Batura and Gopal Rao, 2013; Loeb et al, 2013b; Pepe and Aragona, 2013). At present, men can expect the following rates of toxicity from radical therapies on average: 30% to 90%, erectile dysfunction; 5% to 20%, incontinence; and 5% to 20%, rectal toxicity. Indeed, men may be willing to accept higher rates of genitourinary functional preservation with lower rates of survival. This is reinforced by data from a recent discrete choice experiment showing that men are willing to consider tradeoffs between survival and side effects; for instance, on average men would wish to see 25. First, molecular characterization and imaging modalities may be used to identify men who have high-risk cancer that requires treatment. This has yet to prove fruitful, although imaging is showing some early promise (Kurhanewicz et al, 2008; Macura, 2008; Ahmed et al, 2009a; Turkbey et al, 2009). Second, minimally invasive therapies may be used in an attempt to reduce the side effects of treatment. Although this trend has resulted in intensity-modulated radiotherapy being promoted as the preferred method of care from the radiotherapeutic perspective, on the one hand, and robotic surgery on the other, these treatments are associated with high capital and considerable recurrent costs. Radiotherapy techniques were consistently more expensive than surgery, although both were expensive, with costs ranging from $19,901 (robotic-assisted prostatectomy for low-risk disease) to $50,276 (combined radiotherapy for high-risk disease) (Cooperberg et al, 2013). Others have shown that cost savings are not realized, at least in the first year and in the United States, between open and minimally invasive surgery (Lowrance et al, 2012). Others have shown that proton beam therapy is significantly more expensive, even if it theoretically improves cancer outcomes, compared with photon beam standard radiotherapy (Konski et al, 2007). In addition, there is little robust evidence that the toxicity profile has changed (Sanghani and Mignano, 2006; Berryhill et al, 2008). One way of reducing the side effects of radical therapy may be to direct treatment to only areas of cancer, to preserve tissue and avoid damage to key structures such as neurovascular bundles, external sphincter, bladder neck, and rectum (Ahmed et al, 2007; de la Rosette et al, 2010; Eggener et al, 2010; Lindner et al, 2010b; Karavitakis et al, 2011a).
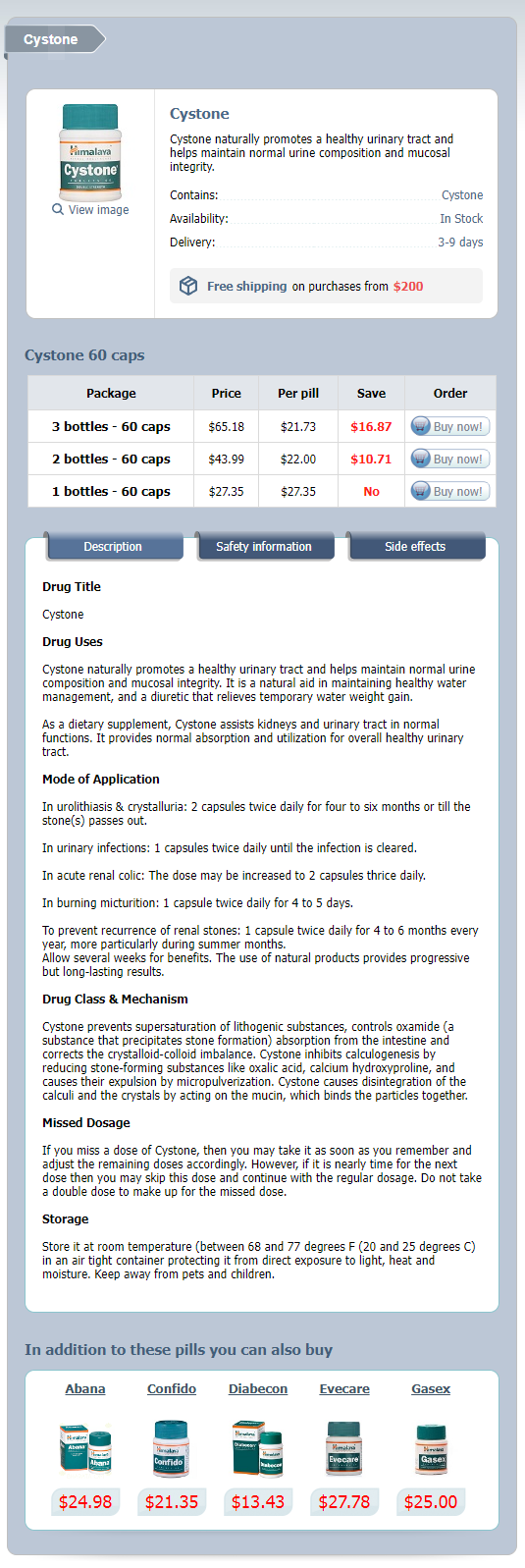
Cystone Dosage and Price
Cystone 60 caps
- 3 bottles - $65.18
- 2 bottles - $43.99
- 1 bottles - $27.35
A comparison of the relative merits of radical perineal and radical retropubic prostatectomy medications kidney stones generic 60caps cystone amex. Early prostate-specific antigen failure following radical perineal versus retropubic prostatectomy: the importance of seminal vesicle excision. Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Preservation of periprostatic autonomic nerves during total perineal prostatectomy by infrafascial dissection. Prospective evaluation of pain medication requirements and recovery after radical perineal prostatectomy. Potency-sparing radical perineal prostatectomy: anatomy, surgical technique and initial results. Perineal approach to radical prostatectomy in kidney transplant recipients with localized prostate cancer. The early diagnosis and radical cure of carcinoma of the prostate: being a study of 40 cases and presentation of a radical operation which was carried out in 4 cases. Patterns of positive specimen margins and detectable prostate-specific antigen after radical perineal prostatectomy. Prospective and longitudinal patient self-assessment of health-related quality of life following radical perineal prostatectomy. These observations provided a more anatomic approach to radical prostatectomy for prostate cancer, resulting in a significant reduction in operative morbidity. Subsequently, the anatomic, nerve-sparing open radical prostatectomy maintained a central role in the management of localized prostate cancer for more than two decades. It was not until 1997 that an attempt at a less invasive approach to radical prostatectomy was explored. In their series of nine patients, operative duration was lengthy (8 to 11 hours) and the length of hospital stay was on average 7. Advances in task-specific surgical instrumentation, optics, digital video equipment, and computer and robotic technology opened a new frontier for minimally invasive laparoscopic prostatectomy. Operative times were in a more acceptable 4- to 5-hour range with reported overall positive margin rates of 15% to 28%. Computer-assisted surgical devices using mechanical robotic arms were adopted for use with radical prostatectomy in part due to their ability to aid the surgeon in performing the challenging task of laparoscopic suturing. By incorporating sophisticated wristed technology at the terminal ends of the robotic instruments, this robotic system offered surgeons the ability to operate, dissect, and suture with the facility of a human wrist. In addition, the 10× magnified, three-dimensional (3D) image provided by the specialized stereo-endoscope lens and camera offered an unprecedented view of the operative field and periprostatic anatomy, far superior to the 2D view of conventional laparoscopy. The first-generation robotic platform, originally launched in the United States in 2000, allowed for the surgeons to control three robotic arms simultaneously, two arms for robotic instrumentation and a third arm for control of the stereo-endoscope and camera. The second-generation da Vinci S system, made available in 2006, incorporated high-definition image capability with an additional fourth robotic arm for grasping and retraction. Issues with equipment expense, the learning curve for the surgeon and surgical team, and patient-related outcomes remain. Patients should have a pathologically confirmed cancer clinically confined within the prostate (stage T1 or T2) or a cancer that extends beyond the margins of the prostate (T3) but still seems amenable to surgical extirpation with a wide resection. Absolute contraindications to minimally invasive laparoscopic prostatectomy include uncorrectable bleeding diatheses and the inability to undergo general anesthesia because of severe cardiopulmonary compromise. In patients with a history of prior laparoscopic extraperitoneal mesh herniorrhaphy, a transperitoneal approach may be preferred over the extraperitoneal approach because dense adhesions in the retropubic space often make attempts at initial access to the space of Retzius challenging. Morbidly obese patients pose additional challenges due to the potential respiratory compromise encountered when placing these patients in a steep Trendelenburg position, as well as the relatively limited working space and limitations of trocar size and instrumentation length. As a result of the effects of prior local radiotherapy or ablation, the tissue planes surrounding the prostate and especially between the posterior prostate and anterior rectum are often fibrotic and obliterated, increasing the risk for inadvertent entry into the rectum during salvage surgery. As a result, patients undergoing salvage prostatectomy need to be counseled on the potential risk for rectal injury and intestinal diversion in addition to the higher incidence of impotence and incontinence compared with surgery in the primary setting. Further discussion regarding the nuances of salvage robotic prostatectomy can be found in the Surgical Techniques section of this chapter. The operation begins by using a 0-degree stereo endoscope and controlling a grasping forceps in the left robotic arm (such as the Maryland curved bipolar forceps or plasma kinetic dissector) and the curved monopolar scissors in the right robotic arm. The fourth robotic arm controls the ProGrasp forceps (Intuitive Surgical), a large atraumatic blunt grasper for retraction and exposure of tissues. The surgeon then toggles between control of any two of the three working robotic arms at any given time to allow for greater autonomy and to achieve optimal exposure and dissection. However, many surgeons have patients use a Fleet enema alone on the morning of surgery. A broad-spectrum antibiotic such as cefazolin is administered intravenously 30 minutes before skin incision. As with open surgery, patients must be counseled on the risk for impotence, incontinence, incisional hernia, and adjacent organ injury. PatientPositioning After induction of general endotracheal anesthesia, the patient is placed in a supine position in steep Trendelenburg with arms and hands carefully tucked and padded at the sides with egg-crate padding to avoid injury to the median and ulnar nerves. The patient is then secured firmly to the table using heavy cloth tape and egg-crate padding across the chest to help prevent the patient from sliding when in the steep Trendelenburg position. Fixed shoulder rests should be avoided because this can result in compression injury to the shoulders and brachial plexus when in steep Trendelenburg. Slight flexion of the table at the level of the hips may be required to properly dock the robotic arms; however, exaggerated flexion should be avoided so as to minimize the risk for femoral neurapraxia (see Complications section). An orogastric tube and urethral catheter are placed to decompress the stomach and bladder, respectively.
© 2025 Adrive Pharma, All Rights Reserved..