General Information about Cleocin
As with any medicine, Cleocin may cause side effects in some individuals. Common unwanted effects could embody diarrhea, nausea, vomiting, stomach ache, and skin rashes. It is essential to consult a doctor if these unwanted effects persist or become severe. In uncommon instances, extra extreme side effects such as severe allergic reactions, liver or kidney harm, and blood issues may happen, and quick medical attention ought to be sought.
One of the significant benefits of Cleocin is that it is obtainable in a quantity of types, making it easier to administer to sufferers. These varieties embody capsules, oral solutions, and injections. The selection of form depends on the severity and placement of the an infection, as well as the affected person's age and medical historical past.
When taking Cleocin, it's important to comply with the dosage and directions offered by the physician rigorously. It is really helpful to take Cleocin with a full glass of water and to space out doses evenly all through the day. Skipping doses or taking higher doses than prescribed can lead to antibiotic resistance and decrease the effectiveness of the medication.
In conclusion, Cleocin is a potent antibiotic used to deal with a variety of serious bacterial infections. Its effectiveness against a broad vary of anaerobic bacteria makes it a useful medicine in the struggle towards bacterial infections. However, it's essential to use it as prescribed and to seek the assistance of with a doctor if any side effects happen. With proper use, Cleocin can effectively treat infections and assist people on the street to recovery.
Cleocin, also referred to as clindamycin, is a powerful antibiotic used to treat serious infections caused by micro organism. It belongs to the lincosamide antibiotic class and is commonly prescribed by medical doctors for a wide selection of bacterial infections.
Cleocin is also generally used in the treatment of infections within the female reproductive system, corresponding to pelvic inflammatory disease, endometriosis, and different infections of the uterus, fallopian tubes, and ovaries. These infections are attributable to quite lots of micro organism, together with anaerobic bacteria.
Anaerobic micro organism are microorganisms that can thrive in environments without oxygen. They could cause severe infections in varied components of the physique, together with the lungs, abdomen, and genital tract. Cleocin works by inhibiting the growth and unfold of these bacteria, allowing the body's immune system to battle off the infection effectively.
In addition to its use in soft tissue and respiratory tract infections, Cleocin can additionally be prescribed for bone and joint infections, such as osteomyelitis and septic arthritis. These types of infections can be difficult to treat and require an extended course of antibiotics. Cleocin is commonly utilized in mixture with other antibiotics in these circumstances to ensure effectiveness.
Cleocin is primarily used to deal with skin infections, respiratory tract infections, bone and joint infections, and infections of the feminine reproductive system. It can be effective in treating severe infections attributable to prone anaerobic bacteria similar to streptococci, pneumococci, and staphylococci.
Cleocin is often prescribed for skin and delicate tissue infections similar to cellulitis, abscesses, and wound infections. These infections are sometimes caused by staphylococci or streptococci, which are kinds of micro organism generally found on the skin. Cleocin can be efficient in treating respiratory tract infections, corresponding to pneumonia, caused by streptococci or pneumococci.
They may present anywhere on the body acne scars purchase 150 mg cleocin with mastercard, but half occur on the oral and genital mucosa. In males, lesions are usually unifocal and can affect the glans or shaft of the penis. Most lesions are 1 to several cm in diameter, but larger plaques may occur, mimicking cellulitis. Histologically, an interface dermatitis occurs with subepidermal vesicle formation, necrosis of keratinocytes, and a mixed superficial and deep infiltrate of neutrophils, eosinophils, and mononuclear cells. Because biopsies are generally performed during the acute stage of a recurrence, the stratum corneum is normal. Papillary dermal fibrosis and deep perivascular pigment incontinence are often present from prior episodes. Barbiturates, tetracyclines, fluconazole, fluoroquinolones, phenolphthalein, acetaminophen, cetirizine, celecoxib, dextromethorphan, hydroxyzine/cetirizine/levocetirizine, quinine, lamotrigine, phenylpropanolamine, erythromycin, metformin, sildenafil, mycophenolate, chemotherapeutic agents, and Chinese and Japanese herbs are also among the long list of possible causes. Patch tests with various concentrations of the offending medication can reproduce the lesion when placed on affected, but not on unaffected, skin Tape-stripping the skin before applying he suspected medication in various vehicles may increase the likelihood of a positive patch test. The pseudocellulitis or scarlatiniform type is characterized by large, tender, erythematous plaques that resolve completely within weeks, only to recur on reingestion of the offending drug. Antibiotics manufactured overseas are readily available in many ethnic markets, including reports of such agents as trimethoprim/sulfamethoxazole in over-the-counter cold medications, and the formulations may not be carefully regulated. In some patients, the reaction may be to a dye in a medication rather than the active ingredient. Fixed drug reaction may rarely be related to foods, including residual antibiotics in meat products and quinine contained in tonic water. Because of the "refractory period," provocation tests need to be delayed at least 2 weeks from the last eruption. Patch testing using a drug concentration of 10%20% in petrolatum or water applied to a previously reacted site is the recommended approach. Tissue resident memory T cells are thought to remain in the skin to provide immunity to infection. The average age in Europe is in the fifties and about one decade younger in Israel and Taiwan. Women have been affected slightly more than men until recently, when a strong female predominance was suggested. The eruption is of sudden onset, within 1 day in many cases associated with antibiotics, and averaging 11 days in other cases. The face and flexural folds are commonly affected first, with ex ension to the trunk and limbs. Facial edema may be seen, and mucous membrane involvement is uncommon, and if present usually affects only one surface and is nonerosive. Laboratory abnormalities typically include a leukocytosis with neutrophilia (90%) and at times an eosinophilia (30%). Characteristically, widespread superficial desquamation occurs as the eruption clears. Hydroxychloroquine is frequently implicated, including in atypical, prolonged courses, but may also induce psoriasis, and it is important to distinguish the two. Chemotherapeutic agents, including small molecule/multikinase inhibitors and other targeted agents, are being reported as inciting agents with increasing frequency. In the classic case, the diagnosis is straightforward, with the characteristic sudden and rapid onset, widespread pustulation, and self-limited course. Due to the severity of the eruption and potential for widespread erythroderma, patients with certain comorbidities may be at risk for complications such as high output heart failure. If there are no characteristic lesions of psoriasis elsewhere and no prior personal or family history of psoriasis, distinguishing these two entities may be impossible, and the patient may need to be followed for a final diagnosis to be made. Histologically, early lesions show marked papillary edema, neutrophil clusters in the dermal papillae, and perivascular eosinophils. The presence of eosinophils and the marked papillary edema help to distinguish this eruption from pustular psoriasis, though pustular psoriasis of pregnancy is often associated with tissue eosinophilia. Patch testing with the suspected agent may reproduce a pustular eruption on an erythematous base at 48 hours in about 50% of patients. In severe cases, cyclosporine, infliximab, or etanercept have rapidly stopped the pustulation and appeared to have hastened the resolution of the eruption. Saénz de Santa Maria García M, et al: Acute generalized exanthematous pustulosis due to diltiazem J Allergy Clin Immunol Pract 2016; 4: 765. Thienvibul C, et al: Five-year retrospective review of acute generalized exanthematous pustulosis. Drug-Induced Pseudolymphoma At times, exposure to medication may result in cutaneous inflammatory patterns that resemble lymphoma. These pseudolymphomatous drug eruptions may resemble either T-cell or B-cell lymphomas. More rarely, medications may induce plaques or nodules, usually in elderly white men after many months of treatment. Importantly, T-cell receptor gene rearrangements in the skin and blood may be positive (or show pseudoclones) in these drug-induced cases, representing a potential pitfall for the unwary physician. Urticarial drug eruptions are the second most common type of cutaneous adverse drug eruption, and can be induced by mmunologic and nonimmunologic mechanisms.
In refractory cases acne 2004 150 mg cleocin for sale, ultrapotent corticosteroids may be used for 23 weeks, then on weekends, with a milder corticosteroid applied during the week. Bexarotene gel can be beneficial in up to 50% of patients with refractory hand eczema. In patients with palmoplantar hyperhidrosis and associated hand eczema, treatment of the hyperhidrosis with intradermal injections of botulinum toxin A leads to both dramatic resolution of the sweating and clearing of the hand eczema. Iontophoresis, which also reduces sweating, can similarly improve hand dermatitis. For example, patients with infrequent but severe outbreaks of pompholyx may benefit from a few weeks of systemic steroids, starting at about 1 mg/kg/day. Patients with persistent, severe hand dermatitis should be considered for alternative, steroid-sparing therapy. The onset of response is delayed, with some patients achieving optimal benefit only after more than 6 months of treatment. Acitretin, may have similar benefit and of course should not be used in women of childbearing potential. The incidence of hand dermatitis in the workplace can be reduced by identifying major irritants and allergens, preventing exposure through engineering controls, substituting less irritating chemicals when possible, enforcing personal protection and glove use, and instituting organized worker education. Hand eczema classes have been documented to reduce the burden of occupational dermatitis. It is important to note that prevention of exposure to a weak but frequent irritant can have more profound effects than removal of a strong but infrequently contacted irritant. Gloves of ethylene vinyl alcohol copolymer sandwiched with polyethylene are effective against epoxy resin, methyl methacrylate, and many other organic compounds. As hospitals transition to nonlatex gloves, it is important to note that even low-protein, powder-free latex gloves reduce self-reported skin problems among health workers. Nonetheless, dermatitis of the diaper area in infants remains a common cutaneous disorder. Diaper dermatitis is also seen in adults with urinary or fecal incontinence who wear diapers. Irritant diaper dermatitis is the most common type of dermatitis and is an erythematous dermatitis due to skin contact with urine and feces that is usually limited to the convex exposed surfaces. The folds remain unaffected, in contrast to intertrigo, inverse psoriasis, and candidiasis, where the folds are frequently involved. In severe cases of irritant dermatitis, there may be superficial erosion or even ulceration (Jacquet erosive diaper dermatitis), violaceous plaques and nodules (granuloma gluteal infantum), or pseudoverrucous papules and nodules; these three entities are part of a disease spectrum and can simulate herpetic infections or genital warts the tip of the penis may become irritated and crusted, with the baby urinating frequently and spots of blood appearing on the diaper. Excessive hydration with maceration of the skin is the primary causal factor in diaper dermatitis. The absence of diaper dermatitis in societies where children do not wear diapers clearly implicates the diaper environment as the cause of the eruption. Many parents will incorrectly switch to cloth diapers when diaper dermatitis occurs even though the superabsorbent modern diapers are much more effective at preventing diaper dermatitis by wicking urine and stool to some extent away from the skin. Bacteria raise the local pH, increasing the activity of fecal lipases and proteases, which leads to more skin breakdown. Candida albicans is frequently a secondary invader and, when present, produces typical satellite erythematous lesions or pustules at the periphery as the dermatitis spreads. Breastfeeding is associated with less frequent diaper dermatitis, and diarrhea is a risk factor. Patients with a chronic localized dermatitis may develop dermatitis at distant sites from scratching or irritating the skin. Autoeczematization (id reaction) refers to the spontaneous development of widespread dermatitis or dermatitis distant from a local inflammatory focus. The agent causing the local inflammatory focus is not the direct cause of the dermatitis at the distant sites. Autoeczematization most frequently presents as a generalized acute vesicular eruption with a prominent dyshidrosiform component on the hands. The most common associated condition is a chronic eczema of the legs, with or without ulceration. The "angry back" or "excited skin" syndrome observed with strongly positive patch tests, and the local dermatitis seen around infectious foci (infectious eczematoid dermatitis), may represent a limited form of this reaction. Patients with a variety of infectious disorders may also present with an id reaction the most classic pattern is characterized by symmetrically distributed minute papules that have a predilection for the face, upper ears, and trunk. The most common causes are tinea capitis or an allergic contact dermatitis Therapy of tinea capi is with griseofulvin can lead to an id reaction soon after therapy that can be mistaken for an allergic reaction to griseofulvin. Proper management is to continue the griseofulvin and treat symptomatically with topical steroids or antihistamines if necessary. Id reactions can also be vesicular on the hands in response to an inflammatory tinea of the feet. Nummular eczematous lesions or pityriasis rosealike lesions may occur in patients with head or pubic louse infestation. Id reactions clear when the focus of infection or infestation is treated, but topical or systemic antiinflammatory agents may be required until the triggering infection is eradicated. A topical corticosteroid spray may be used and will not interfere with appliance adherence. Contact dermatitis to the ostomy bag adhesive can be problematic, and even supposedly hypoallergenic ostomy bags may still trigger dermatitis in these patients. It is estimated that 75% of ileostomy patients have some postoperative sensitivity as a result of the leakage of intestinal fluid onto unprotected skin.
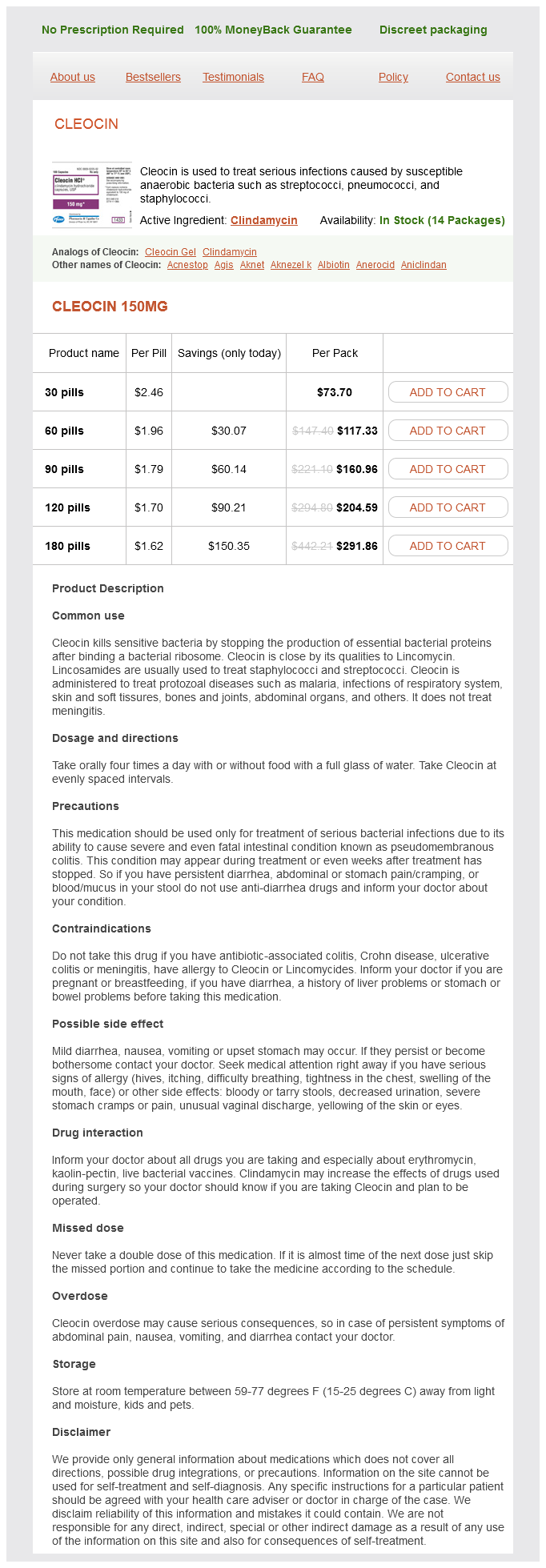
Cleocin Dosage and Price
Cleocin 150mg
- 30 pills - $73.70
- 60 pills - $117.33
- 90 pills - $160.96
- 120 pills - $204.59
- 180 pills - $291.86
A positive diagnosis of allergy at a minimum requires the appearance of a chronic dermatitis after placement acne under microscope buy online cleocin, no other cause, a positive patch test for the suspected metal (or with drug-eluting stents, the drug), and healing after removal. This scenario is exceedingly uncommon; the removal of the foreign material needs to be judged as necessary, reasonable, and safe, and no objective criteria exist to determine the necessity. Dental and gynecologic implants are more frequently replaced; some patients do improve. Patch testing before placement does not seem to predict complications and is therefore not recommended. Because we are all constantly exposed to nickel, nickel dermatitis is a frequent occurrence. A direct relationship between prevalence of nickel allergy and number of pierced sites has been documented. Nickel produces more cases of allergic contact dermatitis than all other metals combined. Black or greenish staining under rings, metal wristbands, bracelets, and clasps is caused by the abrasive effect of cosmetics or other powders containing zinc or titanium oxide on gold jewelry. This skin discoloration is black because of the deposit of metal particles on skin that has been powdered and that has metal, such as gold, silver, or platinum, rubbing on it. Abrasion of the metal results because some powders are hard (zinc oxide) and can abrade the metal. Dimethyl fumarate is highly allergenic, and several outbreaks of shoe dermatitis in Europe have occurred secondary to this allergen. Other causative agents are felt, cork liners, formaldehyde, dyes, asphalt, and tar Shoe refresher sprays may also induce allergy. Patch testing with pieces of various shoe parts may be done by soaking them for 15 minutes in water and applying them to the back for 7296 hours. Once the allergen has been identified, selection of shoes without the offending substance will lead to resolution. Unfortunately, this is a difficult process, because most shoes are made in areas without mandatory labeling requirements, and plastic, wooden, or fabric shoes that contain fewer allergens are often impractical. The snaps on clothing have been implicated in producing allergy in children; nickel is the most common cause of allergic contact dermatitis in children as well as adults. Laptop computers, cell phones, electronic cigarettes, and microneedling devices are newer products capable of causing nickel dermatitis. Metals, including nickel, are increasingly being recognized as a cause of cosmetic allergies. Nickel ranks highly on l sts of occupationally induced allergic contact dermatitis. Piercing the earlobes with nickel-plated instruments or wearing nickel-plated jewelry readily induces nickel sensitivity. Earlobes should be pierced only with stainless steel instruments, and only stainless steel earrings should be worn until the ears have healed. Nickel objects may be plated with chrome but may still cause nickel dermatitis through the leaching of some of the nickel through the small pores of the chromium plating. Homeopathic and complementary medicaments may also contain enough nickel to produce a contact allergy. This affects the degree of nickel dermatitis, being more severe in persons who perspire profusely. Nickel may be detected by applying dimethylglyoxime solution to the test object In the presence of nickel, the cotton swab used to apply the solution will turn orange-pink. A positive test always means that nickel is present, but a negative test does not rule out its presence. Prophylactic measures should include the reduction of perspiration in those sensitive to nickel. Topical corticosteroids applied before exposure to nickel, such as before putting on a wristband, may be successful. Clasps and other objects are available in plastic material so that some of the exposure to nickel may be decreased. Polyurethane varathane 91 applied in three coats will give protection for several months. Treatment of nickel dermatitis consists of the application of topical corticosteroids. In Europe, laws regulating the maximum content of nickel in jewelry have led to a marked decrease in sensitization. Sharon Jacob is leading an effort to have a similar law passed in the United States. Hand eczema and pompholyx in nickel-sensitive or cobaltsensitive patients have rarely been aggravated by ingested metals in the diet. In severe, treatment-resistant dermatitis, a specific diet low in nickel and cobalt may be tried. The chromates are strongly corrosive and irritating to the skin and may act as primary irritants or as sensitizers to produce allergic contact dermatitis. Besides affecting employees in chromate works, chrome dermatitis is encountered among tanners, painters, dyers, photographers, polishers, welders, aircraft workers, diesel engine workers, and those involved with the bleaching of crude oils, tallows, and fats. Traces of dichromates in shoe leather and gloves may cause eczema of the feet and hands. Many zippers are chromium plated, and the nickel underneath may be the causative agent. Matches, hide glues, chrome alloys, cigarette lighters, and leather hatbands, sandals, or camera cases may cause chrome dermatitis. Anticorrosion solutions used for refrigeration and other recirculation systems often contain chromates that produce dermatitis. Most workers in the cement industry who have cement eczema show positive patch tests to dichromates.
© 2025 Adrive Pharma, All Rights Reserved..