General Information about Cialis
In conclusion, Cialis has been a game-changer for males with ED, offering a secure and efficient resolution to enhance erection and achieve successful sexual intercourse. With its longer length of action and more relaxed dosing choices, it has allowed males to regain their sexual confidence and intimacy with their companions. However, it is essential to remember that Cialis is a prescription medication and may solely be taken beneath the steering of a healthcare skilled. With proper use and precautions, Cialis can continue to enhance the sex life of many males and their partners.
Unlike different ED medicines, Cialis has an extended length of motion, lasting as a lot as 36 hours. This implies that men can take the medication properly in advance and it will nonetheless be effective when sexual stimulation happens. This longer window of alternative has given Cialis the nickname 'the weekend pill' as it allows for a extra natural and relaxed approach to sexual activity with out the want to plan for it upfront.
Cialis, also referred to as tadalafil, is a well-liked medicine used to treat erectile dysfunction (ED). It works by increasing blood flow to the penis, thus enhancing erection and helping males obtain successful sexual activity. With hundreds of thousands of males experiencing ED worldwide, Cialis has turn out to be a life-changing medication that has restored intimacy and confidence in relationships.
Cialis for day by day use is taken as quickly as a day, regardless of sexual activity, with a decrease dosage of 2.5 or 5 mg. This is appropriate for men who have regular sexual exercise and want spontaneity in their intercourse life. On the opposite hand, Cialis as needed is taken only when required, at the next dosage of 10 or 20 mg. It is more appropriate for men who've less frequent sexual activity.
Additionally, Cialis has proven to be efficient in men with ED attributable to numerous medical situations. For occasion, males with diabetes, a standard cause of ED, have reported significant improvements of their erectile function whereas taking Cialis. This is due to the medicine's capacity to improve blood circulate to the penis, which is important for reaching and maintaining an erection.
ED is a condition where men are unable to attain or keep an erection sufficient for sexual exercise. It can be brought on by various elements corresponding to stress, anxiety, diabetes, high blood pressure, or even certain medications. Regardless of the trigger, ED can have a significant impression on a man's shallowness and his relationship together with his companion. This is where Cialis is out there in to assist.
Cialis is a phosphodiesterase sort 5 (PDE5) inhibitor, which works by enjoyable the muscle tissue and rising blood circulate to the penis. This action permits for a agency and long-lasting erection, which is critical for successful sexual intercourse. The drug is available in two types: Cialis for every day use and Cialis as needed.
Cialis can additionally be well-tolerated by most males and has a lower risk of side effects compared to other ED medicines. The mostly reported unwanted effects embrace headache, indigestion, back ache, and muscle aches, which are often gentle and subside rapidly. However, it is essential to consult a healthcare professional before taking Cialis to ensure it is protected for you, especially in case you have underlying health situations or take other medicines.
A nonionic flush solution (D5W) is used to flush the system and deliver the agent erectile dysfunction doctor exam cialis 10 mg on line. In order to reduce the number of variables during clinical use, it is probably best to limit oneself to a few ratios of oil to glue (typically 1:1) and become familiar with their behavior. The adhesive is usually injected through a microcatheter either as a series of small depositions (0. Flow control using balloon catheters is sometimes employed but in most situations, it is preferable to use the forward flow of blood to carry the agent deep into the nidus. Careful technique is required to form a cast of the nidus, either by forming a proximal plug of the agent initially or by using a balloon catheter to prevent reflux. Absolute ethanol used intra-arterially in highflow malformations can be a highly effective agent by causing rapid thrombosis and endothelial damage, resulting in permanent occlusion [11, 12]. Due to the toxicity of the agent, it is imperative to confirm that flow will only be into target vessels, as there is a significant risk of tissue damage, including skin sloughing and nerve injury. Small volumes of ethanol are used, with limits on the total dose based on body weight (generally not more than 0. Chapter 48 Interventional Management of Vascular Malformations 427 kg body weight) and the time over which the agent is delivered. Escape of the agent into the central circulation has also been associated with cardiac arrhythmias and acute pulmonary vasoconstriction as well as hemolysis; some authors advocate the routine use of SwanÂGanz monitoring when this agent is used [12]. Treatment is generally recommended even for asymptomatic lesions due to the risk of paradoxical embolization, most seriously resulting in stroke or brain abscess. Multiple or large lesions may also result in arterial desaturation as well as high-output states. As these are virtually always simple fistula-like lesions, cure is possible using macroscopic occluding devices, such as coils, vascular plugs, and detachable balloons. The high flow and low resistance may also result in a clinically significant high-output state. However, the flow through these lesions is torrential, increasing the risk of loss of the embolic device into the pulmonary circulation. These lesions can be approached by arterial embolization, as shown here (C), or by direct puncture of the draining vein. Drainage in this type of lesion is usually into the systemic venous circulation rather than the portal system; treatment is discussed below. Very extensive lesions with rapid shunting may present with high-output cardiac states, including cardiomegaly, shortness of breath or palpitations. Embolization is the most effective treatment for the majority of these patients, as they involve extensive anatomical areas and are generally not amenable to surgical resection. Ligation of feeding vessels is ineffective and makes subsequent treatment more difficult. Superselective embolization of feeding branches will reduce flow and improve symptoms in most patients, and in lesions with a simple blood supply, embolization of the feeding branch may be curative. Probably the most common lesion is the familiar colonic angiodysplasia, a small vessel submucosal malformation generally occurring in the right colon in older patients, often with a history of chronic low-output cardiac states. Depending on the specific anatomy and clinical circumstances, this lesion can be treated surgically or by embolization. These lesions can be complex and difficult to cure completely; acute closure of the shunt also carries the risk of acute portal vein thrombosis which can be fatal. It is probably advisable to embolize these malformations in a staged fashion to avoid this complication. This patient underwent combined arterial and venous embolization for an extensive lesion (A). Although the post angiogram (B) shows no visible residual malformation, she developed massive hematuria from a ruptured draining vein, eventually requiring partial cystectomy. A flush aortogram is performed initially to outline the blood supply to the malformation. Selective study of the major feeders is then carried out to define flow patterns and identify normal branches which need to be preserved. Microcatheters are generally employed for the embolization itself to allow superselective delivery and maintain continued access to the parent vessel for repeated depositions. Except in the case of simple singlevessel lesions, these malformations will generally require multiple sessions to achieve a successful clinical result. An approach which is being used more frequently is a combination of arterial and venous embolization [19, 20]. Occlusion of the venous drainage removes the low pressure sump which tends to cause collateral recruitment and clinical recurrence. This technique is most effective when there is an aneurysmally dilated draining vein which can be accessed either using a catheter from a transvenous approach, or by direct percutaneous puncture of the draining vein. Repeated transcatheter injections into the feeding artery allow progress to be monitored during the embolization procedure. Arteriovenous malformations confined to the uterus generally present with menorrhagia which is often severe. Not only can hysterectomy be avoided, but successful pregnancies have been reported in several patients following embolization. The primary reason for this is the end-circulation nature of the anatomy; it can be much more difficult to define those vessels involved with the malformation as opposed to those necessary for perfusion of normal distal tissues. Often the nidus of the malformation is proximal to the site of clinical manifestations in the extremity, and successfully reducing or eliminating flow through the nidus will result in resolution of the distal problem. As these malformations tend to be diffuse and cross normal tissue planes, resection or even amputation is often not feasible and rarely curative over the long term. Embolization, while itself rarely curative, presents the opportunity to reduce the shunt and improve distal perfusion [24Â26].
In this chapter erectile dysfunction kegel exercises buy 5 mg cialis amex, we have adapted the rating system of the Maudsley staging method for treatment-resistant mania. Specifically, the recognition of sub-syndromal symptoms will alert the clinician to an incomplete recovery and an increased risk of relapse or recurrence. Poor prognostic factors and risk factors for treatment resistance can be grouped as occurring before (delayed diagnosis, earlier age of onset), during (mood incongruent psychotic features, episode duration, mixed episodes, and number of manic episodes), and after (sub-syndromal symptoms, non-adherence) an acute episode. Earlier diagnosis, successful adherence with maintenance treatment, and prompt attention and treatment of psychiatric comorbidities can dramatically improve outcomes in bipolar disorder. Future research directions First, the multi-dimensional model of treatment resistance in mania needs to be tested and validated with existing datasets and future studies, and possibly extended to include mixed episodes. Second, the definitions of treatment resistance need to be extended to maintenance phases of bipolar disorder. Failure of prophylactic treatment or rapid cycling may be associated with additional psychological costs on the medication adherent patient. Only after definitions of treatment resistance in bipolar disorder are established and validated for each phase of the illness will the true prevalence of treatment resistance in bipolar disorder be determined. Factors that limit functional recover shall be further delineated and incorporated in treatment intervention packages. Substance abuse in first-episode bipolar I disorder: indications for early intervention. Safety and efficacy of olanzapine monotherapy in treatment-resistant bipolar mania: a 2-week open-label study. Brief evaluation of medication influences and beliefs: development and testing of a brief scale for medication adherence. A multidimensional tool to quantify treatment-resistance in depression: the Maudsley staging method. Prediction of longer-term outcome of treatment-resistant depression in tertiary care. Diagnosing bipolar disorder and the effect of antidepressants: a naturalistic study. Features associated with the delayed initiation of mood stabilizers at illness onset in bipolar disorder. A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. A meta-analytic investigation of neurocognitive deficits in bipolar illness: profile and effects of clinical state. The effect of anxiety disorder comorbidity on treatment resistant bipolar disorders. Tolerance to the prophylactic effects of carbamazepine and related mood stabilizers in the treatment of bipolar disorders. Evidence-based treatment strategies for treatment-resistant bipolar depression: a systematic review. Mania: differential effects of previous depressive and manic episodes on response to treatment. Two-year syndromal and functional recovery in 29 cases of first-episode major affective disorder with psychotic features. The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. Defining and assessing adherence to oral antipsychotics: a review of the literature. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Chapter 3 Determinants of treatment resistance: health systems and public policy implications Jelena Vrublevska and Konstantinos N Fountoulakis Mood disorders place substantial clinical, social, and economic burden on patients, their families, and the society. Furthermore, affective illnesses are associated with premature death and disability. A large proportion of the burden is likely to be attributable to treatment-resistant mood disorders. Refractory mood disorders themselves are common: treatment resistance is present in 20Â30 per cent of patients (Souery et al. The duration and severity of illness are important determinants of resistance and burden (Ustun and Kessler, 2002). Furthermore, patients with diagnosed mood disorders often have a number of comorbid medical and psychiatric conditions which can have an impact on how patients are managed. Patients with comorbid psychiatric and general medical conditions are more likely to experience functional impairment, and to incur higher mental and medical healthcare costs. The broad economic impact of mood disorders, such as the inability to function fully at work, and the consequent societal productivity losses and social security burden, are sources of increasing concern (Patel, 2009). A number of individuals with mood disorders are not properly diagnosed and therefore do not receive appropriate care. Meanwhile, the scarcity of healthcare resources in some health systems prevents the access to evidence-based treatments. Barriers to improvement of mental health services Notwithstanding the fact that the burden of mental disorders does not vary considerably across countries, recent research indicates that there are large discrepancies between national availability of mental health resources. There is accumulating evidence showing that several countries are unprepared to deal with the predicted worldwide rise in mental and behavioural disorders due to a lack of mental health policies, programmes, and resources. In fact, mental health has a low priority in public health agendas at national and international levels. This has a profound effect, especially on the treatment of refractory cases, which require specialized and collaborative care and closer long-term follow-up. A comparison of data collected in the year 200 with that updated in 2004 had showed a slight increase in countries with a mental health policy, and more countries were providing community mental health services.
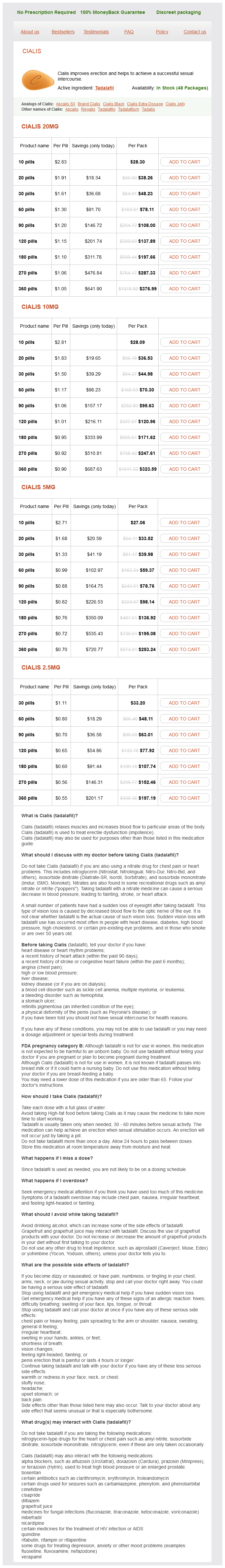
Cialis Dosage and Price
Cialis 20mg
- 10 pills - $28.30
- 20 pills - $38.26
- 30 pills - $48.23
- 60 pills - $78.11
- 90 pills - $108.00
- 120 pills - $137.89
- 180 pills - $197.66
- 270 pills - $287.33
- 360 pills - $376.99
Cialis 10mg
- 10 pills - $28.09
- 20 pills - $36.53
- 30 pills - $44.98
- 60 pills - $70.30
- 90 pills - $95.63
- 120 pills - $120.96
- 180 pills - $171.62
- 270 pills - $247.61
- 360 pills - $323.59
Cialis 5mg
- 10 pills - $27.06
- 20 pills - $33.52
- 30 pills - $39.98
- 60 pills - $59.37
- 90 pills - $78.76
- 120 pills - $98.14
- 180 pills - $136.92
- 270 pills - $195.08
- 360 pills - $253.24
Cialis 2.5mg
- 30 pills - $33.20
- 60 pills - $48.11
- 90 pills - $63.01
- 120 pills - $77.92
- 180 pills - $107.74
- 270 pills - $152.46
- 360 pills - $197.19
Do excimer laser angioplasty and rotational atherectomy facilitate balloon 40 ChaPter 40 Management of Diabetic Foot following Percutaneous Transluminal Angioplasty Laura Kerselaers1 erectile dysfunction middle age 5 mg cialis purchase mastercard, Jьrgen Verbist1, Koen Keirse1, Koen Deloose2, Marc Bosiers2 & Patrick Peeters1 1 2 Imelda Hospital, Bonheiden, Belgium Saint Blasius Hospital, Dendermonde, Belgium Introduction Ischemic diabetic foot ulcers are a challenge to treat because of the aggressive form of atherosclerosis which is typical for this patient population. Up to 70% of all lower leg amputations worldwide are performed on diabetics [1], and of these amputations, up to 85% are preceded by an ulcer [1], which subsequently deteriorates to a severe infection or gangrene [2]. There are many predicting factors in the outcome of diabetic foot ulcers, not only ischemia but also infection control, wound management, pressure relief, neuropathy, and patient comorbidities [1, 2]. These factors explain why it is so important to have meticulous multidisciplinary follow-up after vascular treatment of diabetic foot ulcers [1]. Typical ischemic symptoms are less frequent in diabetic patients, and therefore diagnosis of vascular impairment is often delayed. It is mandatory in the treatment and follow-up of diabetic foot ulcers to consider an underlying ischemic factor unless otherwise proven [2]. Any stagnation or deterioration in ulcer healing after endovascular treatment demands further evaluation and often reintervention [3]. To inform patients of this knowledge is crucial to make them aware of the importance of risk factor modification. But also other factors of aggressive atherosclerotic treatment such as hypertension control, antiplatelet agents, statins, and beta-blocker therapy have been proven to prolong life in this patient population [3, 6]. And last but not least, patients should be educated on the need to contact their doctor as soon as an ulcer reoccurs [1]. A multidisciplinary team should comprise an endocrinologist, a wound care specialist, and a vascular surgeon [3], but other members are indispensable. A podiatrist is important to provide information on preventive footwear, reducing weight bearing, and pressure relief on the ulcer site [7]. It is important that there is no significant infection present when initiating the therapy. Off-loading Diabetic foot ulcers are mostly multifactorial so in ulcers with an important ischemic component, it is crucial not to forget pressure relief as a major step in healing [7]. Nonremovable total-contact casts have been shown to be effective in uncomplicated neuropathic ulcers [6, 7], but they have certain disadvantages, especially in neuroischemic ulcers, because they might reduce activity levels and cause iatrogenic ulcers, and also because they impair the possibility for proper wound care and inspection [16]. Removable walkers, on the other hand, are also effective and do not have the disadvantages of nonremovable casts, but have the problem of poor patient compliance [7, 16]. There are also surgical techniques for off-loading such as metatarsal head resections, Achilles tendon lengthening, metatarsophalangeal joint arthroplasties, and surgical excision of bone segments. These procedures seem to expedite wound healing and reduce ulcer recurrence after revascularization, although more research is still needed [1, 2, 7]. The success rates for off-loading in neuroischemic and/or infected wounds are much lower than in uncomplicated neuropathic wounds, but offloading is perhaps even more important in such complex wounds because these patients are at enhanced risk for limb loss [7]. These are widely used, although they have not been evaluated or compared in carefully designed studies. Important factors in modern wound care include optimizing moisture balance, monitoring the presence of infection and performing debridement for an optimal wound bed [3]. Some studies show benefit for hyperbaric oxygen therapy, but further research is necessary to determine which patients can benefit and what is the optimal duration of therapy [1, 2, 16]. The diagnosis of diabetic foot ulcer infection is based on clinical findings such as purulent secretion in the ulcer or a sinus tract, or two or more of the following symptoms: erythema, warmth, swelling, tenderness, bad odor, or increased exudation rate [2, 14, 16]. If infected ulcers are complicated by abscess, extensive bone or joint involvement, gangrene, or 350 Pa r t 2 Peripheral Interventions necrotizing fasciitis, urgent surgical incision and drainage and radical debridement are the most important steps in controlling deep infection [2, 14]. Studies have confirmed a significantly lower rate of above-ankle amputation in cases of early surgical debridement [14]. Prior to starting empirical antibiotic therapy, it is important to take deep wound cultures, obtained by biopsy, curettage of an ulcer base, or aspiration from an abscess, instead of superficial wound swab specimens [2, 14, 16]. Mild-to-moderate infections can often be treated with a relatively narrow-spectrum antibiotic agent, covering aerobic gram-positive cocci, such as clindamycin or amoxicillin/clavulanate, given orally. Moderate-to-severe infections should be treated intravenously with broad-spectrum antibiotics, also covering aerobic gram-negative bacilli and anaerobes, such as clindamycin plus ciprofloxacin or piperacillin/tazobactam [14, 17]. In deciding which antibiotic therapy to use, the following factors should be considered: severity of infection, history of recent antibiotic treatment, previous infection with resistant organisms, recent culture results, and patient factors [17]. Antibiotic therapy should be continued until the infection has resolved, but not necessarily for the entire duration that the wound stays open [2, 14]. The risk for osteomyelitis is substantial in ulcers with visible bone or an ability to probe bone, or an ulcer size larger than 2 Ч 2 cm. Magnetic resonance imaging and a bone scan can be useful in diagnosis of the disease, especially in deciding on type and duration of antibiotic therapy [2, 14, 16]. Vascular follow-up Clinical vascular follow-up is not sufficient in ischemic diabetic foot ulcers because of several different reasons. First, symptoms of rest pain are far less common than in nondiabetics, probably due to peripheral neuropathy, which impairs sensory feedback [18]. Second, even with impaired perfusion, the diabetic foot may appear pink and relatively warm due to arteriovenous shunting [2]. Instead, toe pressure measurement is often recommended because it is more accurate in diabetics, since digital vessels are usually spared from calcifications [18]. However, toe pressure measurements are not widely used, because they require appropriate technique and small cuffs. Furthermore, it may be impossible to perform toe pressure measurements in patients with inflammatory ulcerations of their toes or a previous amputation of the big toe [2, 18]. The current imaging options for vascular follow-up also have important limitations in ischemic diabetic foot follow-up. Although there have been recent developments, infrapopliteal imaging remains technically demanding because of the longitudinal anatomy combined with small diameter vessels [3, 18, 20, 21].
© 2025 Adrive Pharma, All Rights Reserved..