General Information about Cialis Soft
Apart from being an efficient treatment for ED, Cialis Soft additionally has a good safety profile. As with any medicine, there's a danger of side effects, but they're usually delicate and transient, including headache, heartburn, back ache, and muscle aches. Most of these side effects are probably to subside because the physique will get used to the medication.
The lively ingredient in Cialis Soft is Tadalafil, which belongs to a gaggle of medicines known as phosphodiesterase sort 5 (PDE5) inhibitors. This treatment works by growing blood flow to the penis, which helps to maintain an erection throughout sexual stimulation. It also relaxes the sleek muscle tissue within the blood vessels, permitting for elevated blood move to the penis, resulting in a profitable erection.
Cialis Soft has been shown to be efficient in serving to males with ED obtain and preserve an erection. According to a research printed within the Journal of Sexual Medicine, sufferers taking Cialis Soft reported a major improvement in erectile operate, with 60% of them reporting that they had been in a place to have a successful sexual activity in comparison with only 30% of these taking a placebo.
Cialis Soft is a well-liked treatment that is generally used to deal with erectile dysfunction (ED) in men. Unlike conventional Cialis, Cialis Soft comes in a chewable pill form, making it easier and faster to soak up in the physique. This medication has gained a big amount of popularity due to its effectiveness in treating ED and helping men achieve a profitable sexual activity.
One of the important thing advantages of Cialis Soft is its quick absorption price. As it is obtainable in a chewable form, it is easier for the body to dissolve the tablet, making it enter the bloodstream faster than traditional Cialis. This means that the consequences of the medication can be felt within 15-20 minutes, in comparison with the 30 minutes to an hour for conventional Cialis. This makes Cialis Soft an ideal alternative for males who want to have a spontaneous sexual encounter with out having to wait for a really lengthy time for the medication to take effect.
It is essential to note that Cialis Soft is a prescription medication and will only be taken underneath the steering of a healthcare provider. It just isn't meant for everybody, particularly those who have a history of coronary heart issues, liver or kidney illness, and these who are currently taking nitrates for chest ache. Taking Cialis Soft along with these drugs can lead to a sudden drop in blood stress, which may be harmful.
In conclusion, Cialis Soft is a extremely efficient and handy therapy for ED. It has a fast onset of action, long length of effect, and has a good security profile. With its chewable form and longer length, it is an ideal choice for men who wish to improve their sexual performance and have a more fulfilling sex life. However, it's imperative to seek the advice of a healthcare professional earlier than taking this medication to ensure it is protected and appropriate for you.
Another advantage of Cialis Soft is its longer period of motion. This medicine can last up to 36 hours, giving males the flexibleness to engage in sexual exercise at any time during this period. This long-lasting effect is for much longer in comparison with other ED medications, making it a most popular choice for so much of people.
These criteria are useful for selecting patients for bronchoscopic or nonbronchoscopic procedures that yield lower respiratory tract samples protected from upper-tract contamination; quantitative cultures of such specimens have diagnostic sensitivities in the range of 80% do erectile dysfunction pumps work buy cialis soft paypal. Second, early-onset nosocomial pneumonia, which manifests within the first 4 days of hospitalization, is most often caused by community-acquired pathogens such as Streptococcus pneumoniae and Haemophilus species, although some studies have challenged this view. Third, one multicenter study suggested that 8 days is an appropriate duration of therapy for nosocomial pneumonia and lessened emergence of resistant pathogens. Fourth, a controversial study of health careassociated pneumonia suggested that therapy based on guidelines from professional societies did not improve patient outcomes. Finally, in febrile patients (particularly those who have tubes inserted through the nares), occult bacterial sinusitis and otitis media should be considered. The average wound infection has an incubation period of 57 days-longer than many postoperative stays. For this reason and because many procedures are now performed on an outpatient basis, the incidence of wound infections has become more difficult to assess. True airborne spread of infection through droplet nuclei is rare in operating rooms unless there is a disseminator. Additional risks include the presence of drains, prolonged preoperative hospital stays, shaving of operative sites by razor the day before surgery, long duration of surgery, and infection at remote sites. Reporting surveillance results to surgeons has been associated with reductions in infection rates. The process of diagnosing and treating wound infections begins with a careful assessment of the surgical site. Diagnosis of infections of prosthetic devices, such as orthopedic implants, may be complicated when pathogens are cloistered in prosthesis-adherent biofilms; cultures of sonicates from explanted prosthetic joints have been more sensitive. In rapidly progressing postoperative infections manifesting within 2448 h of a surgical procedure, the level of suspicion regarding group A streptococcal or clostridial infection (Chaps. National estimates have indicated that ~72,000 primary bloodstream infections occur in the United States each year. With increasing care of seriously ill patients in the community, vascular catheterassociated bloodstream infections acquired in outpatient settings are becoming more frequent. Catheter-related bloodstream infections derive largely from the cutaneous microflora of the insertion site, with pathogens migrating extraluminally to the catheter tip, usually during the first week after insertion-a risk that has been lessened greatly by use of bundled catheter-insertion guidelines. Intrinsic (during the manufacturing process) or extrinsic (on-site in a health care facility) contamination of infusate, although rare, is the most common cause of epidemic device-related bloodstream infection. The most common pathogens isolated from vascular device associated bacteremias include coagulase-negative staphylococci, S. Many pathogens, especially staphylococci, produce extracellular polysaccharide biofilms that facilitate attachment to catheters and provide sanctuary from antimicrobial agents. Vascular devicerelated infection is suspected on the basis of the appearance of the catheter site or the presence of fever or bacteremia without another source in patients with vascular catheters. The diagnosis is confirmed by the recovery of the same species of microorganism from peripheral-blood cultures (preferably two samples drawn from peripheral veins by separate venipunctures) and from semiquantitative or quantitative cultures of the vascular catheter tip. Therapy for vascular accessrelated infection is directed at the 1027 pathogen recovered from the blood and/or infected site. Important considerations in treatment are the need for an echocardiogram (to evaluate the patient for endocarditis), the duration of therapy, and the need to remove potentially infected catheters. In one report, approximately one-fourth of patients with intravascular catheterassociated S. Standard precautions are designed for the care of all patients in hospitals and aim to reduce the risk of transmission of microorganisms from both recognized and unrecognized sources. These precautions include gloving and hand cleansing for potential contact with (1) blood; (2) all other body fluids, secretions, and excretions, whether or not they contain visible blood; (3) nonintact skin; and (4) mucous membranes. Depending on exposure risks, standard precautions also include use of masks, eye protection, and gowns. Precautions for the care of patients with potentially contagious clinical syndromes. Sets of precautions may be combined for diseases that have more than one route of transmission. Some prevalent antibiotic-resistant pathogens, particularly those that colonize the gastrointestinal tract. Wearing gloves does not replace the need for hand hygiene because hands sometimes (in up to 20% of interactions) become contaminated during wearing or removal of gloves. To further lessen the risk of self-contamination, some personnel shun ties and long-sleeves, a practice that is understandable although not scientifically supported as a means of reducing the spread of resistant bacteria. Control of seasonal influenza has depended on (1) the use of effective vaccines, with increasingly broad evidence-based recommendations for vaccination of children, the general public, and health care workers; (2) the use of antiviral medications for early treatment and for prophylaxis as part of outbreak control, especially for high-risk patients and in high-risk settings like nursing homes or hospitals; and (3) infection control (surveillance and droplet precautions) for symptomatic patients. Controversial infection-control issues have been the questionable role of airborne spread of influenza and the historical embarrassingly low rates of vaccination among health care workers, which have now markedly improved, in part as a result of mandated vaccination policies in many hospitals. In the spring of 2009, a novel strain of influenza virus-H1N1 (swine flu) virus-caused the first influenza pandemic in four decades. For now, control measures include judicious use of all antibiotics, especially fluoroquinolone antibiotics that have been implicated in driving outbreaks; heightened suspicion for atypical presentations. To improve diagnosis, use of more sensitive polymerase chain reactionbased rather than enzyme immunoassaybased testing of diarrheal stool is now recommended, with resultant artificial doubling of infection rates (as patients who are colonized but not clinically infected with C. Preliminary data suggest a role for probiotics in the prevention of diarrhea in patients in whom systemic antibiotic therapy is being initiated. Fecal transplantation has had dramatic results in the treatment of relapsing cases of C. Successes with fecal transplants and probiotics have called attention to the potential role of manipulation of the intestinal microbiome as a broader infection-control strategy.
One of the most common hemophilia A mutations results from an inversion of the intron 22 sequence impotence effect on relationship buy 20 mg cialis soft otc, and it is present in 40% of cases of severe hemophilia A. Advances in molecular diagnosis now permit precise identification of mutations, allowing accurate diagnosis of women carriers of the hemophilia gene in affected families. In the severe and moderate forms, the disease is characterized by bleeding into the joints (hemarthrosis), soft tissues, and muscles after minor trauma or even spontaneously. Patients with mild disease experience infrequent bleeding that is usually secondary to trauma. Early in life, bleeding may present after circumcision or rarely as intracranial hemorrhages. In the severe form, the most common bleeding manifestations are the recurrent hemarthroses, which can affect every joint but mainly affect knees, elbows, ankles, shoulders, and hips. Acute hemarthroses are painful, and clinical signs are local swelling and erythema. To avoid pain, the patient may adopt a fixed position, which leads eventually to muscle contractures. Very young children unable to communicate verbally show irritability and a lack of movement of the affected joint. Chronic hemarthroses are debilitating, with synovial thickening and synovitis in response to the intraarticular blood. After a joint has been damaged, recurrent bleeding episodes result in the clinically recognized "target joint," which then establishes a vicious cycle of bleeding, resulting in progressive joint deformity that in critical cases requires surgery as the only therapeutic option. Hematomas into the muscle of distal parts of the limbs may lead to external compression of arteries, veins, or nerves that can evolve to a compartment syndrome. Retroperitoneal hemorrhages can accumulate large quantities of blood with formation of masses with calcification and inflammatory tissue reaction (pseudotumor syndrome) and also result in damage to the femoral nerve. Hematuria is frequent among hemophilia patients, even in the absence of genitourinary pathology. The availability of factor concentrates resulted in a dramatic improvement in life expectancy and in quality of life for people with severe hemophilia. Factor replacement therapy for hemophilia can be provided either in response to a bleeding episode or as a prophylactic treatment. Primary prophylaxis is 832 defined as a strategy for maintaining the missing clotting factor at levels ~1% or higher on a regular basis in order to prevent bleeds, especially the onset of hemarthroses. The Centers for Disease Control and Prevention reported that 51% of children with severe hemophilia who are aged <6 years receive prophylaxis, increasing considerably from 33% in 1995. Prophylaxis is the standard care for children; however, teenagers and young adults do not always maintain the treatment regularly. Although highly recommended, the high cost and difficulties in accessing peripheral veins in young patients and the potential infectious and thrombotic risks of long-term central vein catheters are important limiting factors for many young patients. General considerations regarding the treatment of bleeds in hemophilia include the following: (1) Treatment should begin as soon as possible because symptoms often precede objective evidence of bleeding; because of the superior efficacy of early therapeutic intervention, classic symptoms of bleeding into the joint in a reliable patient, headaches, or automobile or other accidents require prompt replacement and further laboratory investigation. In specific situations such as after surgery, continuous infusion of factor may be desirable because of its safety in achieving sustained factor levels at a lower total cost. Mild bleeds such as uncomplicated hemarthroses or superficial hematomas require initial therapy with factor levels of 3050%. Additional doses to maintain levels of 1525% for 2 or 3 days are indicated for severe hemarthroses, especially when these episodes affect the "target joint. Prophylactic replacement for surgery is aimed at achieving normal factor levels (100%) for a period of 710 days; replacement can then be tapered depending on the extent of the surgical wounds. Oral surgery is associated with extensive tissue damage that usually requires factor replacement for 13 days coupled with oral antifibrinolytic drugs. The duration of the treatment depending on the clinical indication is 1 week or longer. These drugs are not indicated to control hematuria because of the risk of formation of an occlusive clot in the lumen of genitourinary tract structures. Inhibitors usually appear early in life, at a median of 2 years of age, and after 10 cumulative days of exposure. However, intensive replacement therapy such as for major surgery, intracranial bleeding, or trauma increases the risk of inhibitor formation for patients of all ages and degree of clinical severity, which requires close laboratory monitoring in the following weeks. The clinical diagnosis of an inhibitor is suspected when patients do not respond to factor replacement at therapeutic doses. Because early detection of an inhibitor is critical to a successful correction of the bleeding or to eradication of the antibody, most hemophilia centers perform annual screening for inhibitors. The Bethesda assay uses a similar principle and defines the specificity of the inhibitor and its titer. Clinically, inhibitor patients are classified as low responders or high responders, which provides guidelines for optimal therapy. Therapy for inhibitor patients has two goals: the control of acute bleeding episodes and the eradication of the inhibitor. For eradication of the inhibitory antibody, immunosuppression alone is not effective. Although this therapy may reduce the inhibitor titers in some cases, sustained eradication is uncommon. Gene therapy trials for hemophilia A and B using adenoassociated viral vectors are ongoing (Chap. The comorbidity of the underlying liver disease in hemophilia patients is clear when these individuals require invasive procedures; correction of both genetic and acquired (secondary to liver disease) deficiencies may be needed. The life expectancy of a patient with severe hemophilia is only ~10 years shorter than the general male population. In patients with mild or moderate hemophilia, life expectancy is approaching that of the male population without coagulopathy. Early data indicate that mortality from coronary artery disease is lower in hemophilia patients than the general male population.
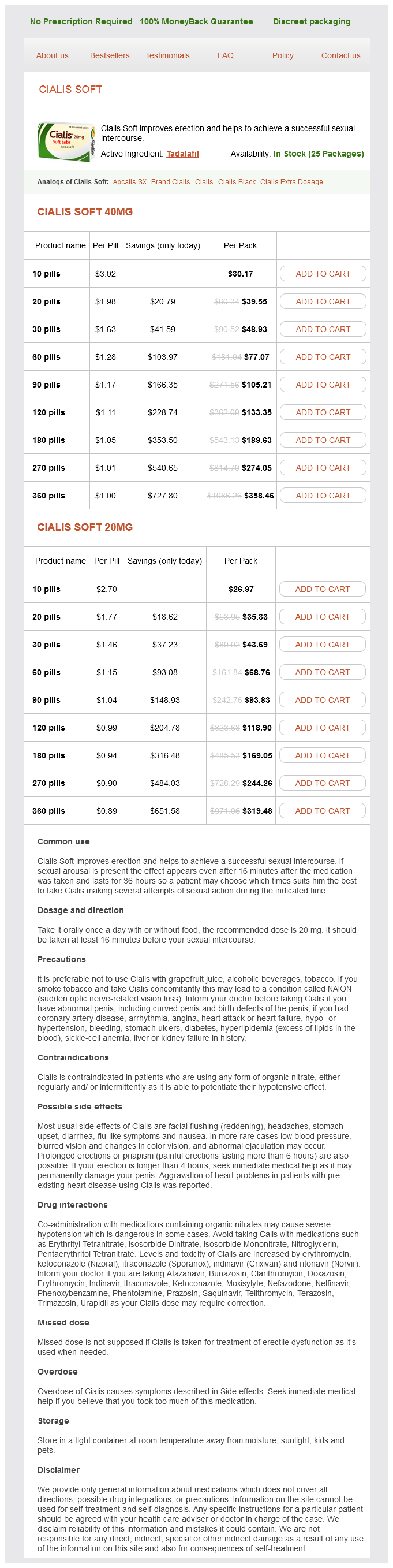
Cialis Soft Dosage and Price
Cialis Soft 40mg
- 10 pills - $30.17
- 20 pills - $39.55
- 30 pills - $48.93
- 60 pills - $77.07
- 90 pills - $105.21
- 120 pills - $133.35
- 180 pills - $189.63
- 270 pills - $274.05
- 360 pills - $358.46
Cialis Soft 20mg
- 10 pills - $26.97
- 20 pills - $35.33
- 30 pills - $43.69
- 60 pills - $68.76
- 90 pills - $93.83
- 120 pills - $118.90
- 180 pills - $169.05
- 270 pills - $244.26
- 360 pills - $319.48
Antibodies with these biphasic properties are called Donath-Landsteiner antibodies erectile dysfunction injection drugs 20 mg cialis soft purchase overnight delivery. The P antigen is the cellular receptor of parvovirus B19 and also may be a receptor for Escherichia coli binding to urothelial cells. Anti-S and anti-s IgG antibodies may develop after pregnancy or transfusion and lead to hemolysis. Such occurrence is problematic; virtually every donor is incompatible because nearly all persons express U. The Kell protein is very large (720 amino acids), and its secondary structure contains many different antigenic epitopes. Such individuals can produce an anti-Kx antibody that makes finding a compatible blood product difficult. The Duffy antigens are codominant alleles, Fya and Fyb, that also serve as receptors for Plasmodium vivax. Additional typing for other main Rh antigens (CcEe), the K antigen, and more rarely Duffy, Kidd and Ss antigens, can be required depending on the clinical setting. The specificity of the alloantibody is identified by correlating the presence or absence of antigen with the results of the agglutination. In the setting of a systematic alloantibody screen, such a crossmatch can be restricted to alloimmunized patients as well as patients at high risk of alloimmunization (prior pregnancies, transfusions). Nonreactive cross-matching confirms the absence of any major incompatibility and reserves that unit for the patient. In the case of Rh (D) -negative patients, every attempt must be made to provide Rh-negative blood components to prevent alloimmunization to the D antigen. In an emergency, Rh-positive blood can be safely transfused to an Rh-negative patient who lacks anti-D; however, the recipient is likely to become alloimmunized and produce anti-D. Blood products intended for transfusion are routinely collected as whole blood (450 mL) in various anticoagulants. The buffy coat then undergoes pooling and is centrifuged at low speed to produce pooled platelets. The leukocyte level of blood products can be lowered by an additional filtration step after which they are referred to as leukoreduced (or leukodepleted) (<1 to 5 × 106 leukocytes per product). Apheresis technology is used for the collection of multiple units of platelets from a single donor. It is the ideal component for patients who have sustained acute hemorrhage of 25% total blood volume loss. Whole blood is stored at 4°C to maintain erythrocyte viability, but platelet dysfunction and degradation of some coagulation factors occur. In addition, 2,3bisphosphoglycerate levels fall over time, leading to an increase in the oxygen affinity of the hemoglobin and a decreased capacity to deliver oxygen to the tissues, a problem with all red cell storage. Fresh whole blood avoids these problems, but it is typically used only in emergency settings. Whole blood is not readily available, since it is routinely processed into components. Adequate oxygenation can be maintained with a hemoglobin content of 70 g/L in the normovolemic patient without cardiac disease; however, comorbid factors may necessitate transfusion at a higher threshold. The decision to transfuse should be guided by the clinical situation and not by an arbitrary laboratory value. In the critical care setting, liberal use of transfusions to maintain near-normal levels of hemoglobin has not proven advantageous. In most patients requiring transfusion, levels of hemoglobin of 80 g/L are sufficient to keep oxygen supply from being critically low. The majority of cellular blood products are now leukocyte-reduced and universal prestorage leukocyte reduction has been recommended. Prestorage filtration appears superior to bedside filtration as smaller amounts of cytokines are generated in the stored product. Plasma, which may cause allergic reactions, can be removed from cellular blood components by washing. Platelets are stored in plasma or in additive solution up to 57 days at 2024°C and under permanent motion. In patients without fever or infections, a threshold of 5000/L may be sufficient to prevent spontaneous hemorrhage. Patients who may require multiple transfusions are best served by receiving leukocyte-reduced components to lower the risk of alloimmunization. Adverse reactions to transfused blood components occur despite multiple tests, inspections, and checks. Fortunately, the most common reactions are not life threatening, although serious reactions can present with mild symptoms and signs. Some reactions can be reduced or prevented by modified (filtered, washed, or irradiated) blood components. When an adverse reaction is suspected, the transfusion should be stopped and reported to the blood bank for investigation. Immune-mediated reactions are often due to preformed donor or recipient antibody; however, cellular elements may also cause adverse effects. Nonimmune causes of reactions are due to the chemical and physical properties of the stored blood component and its additives. Transfusion-transmitted viral infections are increasingly rare due to improved screening and testing.
© 2025 Adrive Pharma, All Rights Reserved..