General Information about Cefuroxime
Apart from these widespread infections, Ceftin can also be used to treat urinary tract infections (UTIs), which can occur within the bladder, kidneys, or urethra. UTIs are generally caused by micro organism coming into the urinary tract, and Ceftin effectively targets these micro organism, relieving the discomfort and burning sensation skilled by sufferers. Additionally, Ceftin can be used to treat Lyme illness, a bacterial an infection transmitted via tick bites, and gonorrhea, a sexually transmitted infection.
Cefuroxime, generally identified by its model name Ceftin, is an antibiotic medication used for treating numerous bacterial infections. This powerful medicine belongs to a bunch of antibiotics generally identified as cephalosporins and is specifically classified as a second-generation cephalosporin. It is primarily used for treating infections in the respiratory system, urinary tract, skin, and ears, making it a flexible and important drug within the medical subject.
In conclusion, Ceftin is a highly effective medication that has proven to be a go-to for varied bacterial infections. It offers quick and environment friendly relief from symptoms, promoting a speedy restoration. However, it is essential to use this treatment responsibly and with warning to avoid any potential side effects or drug resistance. Always consult a health care provider earlier than beginning any medication, and observe their directions for the finest possible consequence.
As with any medication, there are some precautions that need to be taken whereas utilizing Ceftin. It is essential to disclose any known allergic reactions or other underlying medical situations to the prescribing physician to avoid any opposed reactions. Pregnant or lactating girls must also seek the advice of their physician before taking Ceftin. Additionally, it is essential to finish the complete course of antibiotics prescribed, even when you begin feeling higher after a few days. Stopping the treatment prematurely could lead to the formation of antibiotic-resistant micro organism, making it tougher to treat the infection in the future.
In addition to sinus infections, Ceftin is also efficient in treating pores and skin infections like cellulitis and impetigo. These skin infections are brought on by bacteria penetrating the skin's outer layer, resulting in irritation, redness, and pain. Ceftin successfully tackles these infections and prevents them from spreading, thus promoting quick and environment friendly therapeutic.
One of the most common makes use of of Ceftin is for sinus infections, that are caused by micro organism coming into the sinus cavities and inflicting inflammation. The symptoms of a sinus an infection can be quite uncomfortable, together with a blocked nostril, headaches, and facial ache. Ceftin effectively targets the bacteria and relieves the symptoms, providing reduction to the patient.
Furthermore, Ceftin can be helpful in treating infections in the respiratory system, such as pneumonia, bronchitis, and tonsillitis. These infections may be caused by a wide selection of bacteria, and Ceftin targets them all, providing relief from signs like coughing, difficulty breathing, and sore throat. Ceftin is also effective in treating ear infections, which could be fairly common, especially amongst kids. By concentrating on the micro organism causing the an infection, Ceftin reduces the irritation and discomfort, permitting for a speedy restoration.
Ceftin belongs to the household of antibiotics which are similar to penicillin and works by interfering with the formation of the bacterial cell wall, thereby stopping the bacteria from rising and multiplying. This, in flip, results in the eventual death of the micro organism, thus curing the infection. The treatment is on the market in oral type, as tablets and suspensions, making it handy to use and simply accessible to patients.
This conclusion was supported by the findings of a systematic review (search dates medications just for anxiety buy cefuroxime 500 mg cheap, 1966-1997) published in 1999. In these studies, pregnant women were treated with spiramycin alone, pyrimethamine/sulfonamide, or with a combination of both, and the rate of infection in the fetus was assessed; however, gestational stage was not adequately controlled, treatment was not randomized, and the untreated controls were generally not directly comparable to the treatment groups. Five of these studies reported significantly lower transmission rates in children born to treated mothers, and four reported no reduction in fetal infection. An additional study was included in an updated version of the review, but the overall level of evidence in favor of treatment remained low. This comparison failed to find that more intensive treatment was more effective in terms of risk prevention than no or shorter treatment. First, maternal infections are often asymptomatic, and their incidence is low-less than 1% in the majority of studies (see "Infection in Pregnant Women"). As a consequence, the effectiveness of antenatal treatment on transmission can only be assessed in the context of mass screening involving a large number of patients. Second, proving the absence of infection in all uninfected children and detecting 100% of infected children requires a 1-year postnatal follow-up to monitor the clearance or persistence of IgG antibodies, and the organization of such a follow-up for a large group of newborns requires substantial effort and resources. Third, the risk of transmission is relatively low during the first and second trimesters when the incidence of fetal lesions, which are of interest for the reduction of severity, is highest. Fourth, measuring the impact of treatment on the onset of sequelae later in life requires the extension of clinical follow-up far beyond birth for all infected children. Therefore, the fifth challenge for assessing the efficacy of prenatal treatment is to take postnatal interventions into account, although they might not be as effective as prenatal interventions. It is important to control for this variable to avoid confounding,513 which is best achieved with a randomized, controlled study design. This change in screening was associated with a significantly faster initiation of antenatal treatment after mid-1992 (P <. These findings provide indirect evidence that early treatment can reduce transmission (Table 31-19) but do not indicate to what extent, compared with no treatment. Therefore they do not replace the need for randomized controlled studies to evaluate the efficacy of existing regimens or to compare the efficacy of new with that of existing treatments. Priority should be given to carrying out these trials in settings where infections are most severe because of virulent strains and/or increased host susceptibility. First is the ability to generalize conclusions from the findings in Europe to other settings. These conclusions could probably be extrapolated to North America, as discussed in several publications. However, because follow-up testing was rarely performed, a majority of infections were diagnosed at the first test during the first trimester. This overrepresentation of early infections and the impossibility of excluding that some were acquired before pregnancy prevented a fair comparison with the higher rate found in France in the context of the monthly follow-up testing program. A survey performed on 34,000 pregnant women in France suggested that as many as 80% were not consistently 1. If it was determined that such treatment was not beneficial, cessation of this practice could alleviate human and financial costs. The early treatment of an infected fetus is expected to reduce the risks of immediate and long-term lesions of toxoplasmosis. In the absence of data from controlled trials, the available evidence is derived from observational studies, which were not designed to address the efficacy of treatment. In the absence of comparable control groups, it was impossible to attribute any observed benefits solely to the administration of prenatal treatment in the vast majority of these studies. Further confounding interpretation, the few untreated mothers in such studies were also the least likely to give birth to a child with an overt infection because they acquired infections in the last trimester of pregnancy, and the risk for neurologic signs was typically predicted by gestational stage at the time of maternal infection, rather than by the absence of treatment. Some reports also provided information on the postnatal outcome, but, except for a few cohorts, the median length of follow-up did not extend beyond early childhood. In several noncontrolled studies, a different approach, based on the association between treatment delay and risk of infection, provided indirect evidence suggesting that prenatal treatment reduces the risk of lesions in utero or during the first 3 years of life. This risk was not found to be reduced by treatment with pyrimethamine/sulfonamide compared with spiramycin alone or increased by a delay in the administration of treatment, but the power to detect both associations was limited. The effect of pyrimethamine and sulfonamide alone or after spiramycin was similar to that of spiramycin alone. The risk of ocular lesions at 12 months of age was not found to be increased when prenatal treatment was delayed by more than 4 weeks after the estimated gestational stage at the time of maternal infection. The proportion of live-born infected children who had been diagnosed as being infected antenatally was greater after 1995 (87/272, 32. In addition, the probabilities of clinical signs developing in live-born children (either uninfected or, when infected, followed for 3 years) were significantly lower in infected children born to mothers who were diagnosed after 1995 than those who were diagnosed before 1995 (46/1150 vs. Those carried out in the United States on newborns, whose infections were detected because of an overt infection and not through an organized screening program, provided the greatest amount of information. In this context, postnatal treatment was primarily aimed at reducing neurologic impairment and attempting to prevent new retinochoroidal lesions. Despite the absence of concurrent comparative studies, these provided indirect evidence of a positive effect of a 12-month treatment with pyrimethamine and sulfadiazine on neurologic prognosis457,466,946 (see "Management of Congenitally Infected Children and Long-Term Outcome"). Two cohort studies published in 2008 suggested that postnatal treatment might also have an impact on the risk of long-term ocular lesions. The first included 108 patients who had received 12 months of treatment with pyrimethamine and sulfadiazine after birth,936 whereas the second included 25 patients who were not treated in their first year of life despite probable congenital infection.
Infants born at 35 or more weeks of gestation who appear healthy and whose mothers received intrapartum prophylaxis with penicillin symptoms gallbladder problems purchase cefuroxime 500 mg overnight delivery, ampicillin, or cefazolin for 4 or more hours before delivery do not have to be evaluated or treated but should be observed in the hospital for 48 hours. Infants who are less than 35 weeks of gestation, who appear healthy, and whose mothers received penicillin, ampicillin, or cefazolin for less than 4 hours before delivery should receive a limited evaluation, including a blood culture and a complete blood cell count with a differential count, and be observed for 48 hours in the hospital. The first two clinical scenarios are readily identified, but the third category often leads to controversy regarding optimal management. Management of the infant born to a mother who received an antimicrobial agent within hours of delivery must include consideration of the effect of the drug on cultures obtained from the infant after birth. If the infant is infected and the bacterial pathogen is susceptible to the drug administered to the mother, cultures of the infant can be sterile despite a clinical course suggesting sepsis. If the neonate appears to be well and there is reason to believe that infection was unlikely, treatment can be discontinued at 48 hours. If the clinical condition of the infant remains uncertain and suspicion of an infectious process remains, therapy should be continued as outlined for documented bacterial sepsis unless another diagnosis becomes apparent. Squire and colleagues651 found that results of premortem blood cultures were negative in 7 (18%) of 39 infants with unequivocal infection at autopsy. Some infants with significant systemic bacterial infection may not be identified by the usual single blood-culture technique. The physician must consider this limitation when determining length of empirical therapy. However, if treatment for infection is deemed necessary, parenteral administration for 10 days is recommended. The goal of the Duke study was to evaluate the relationship between central venous 6 · Bacterial Sepsis and Meningitis 251 catheter removal and outcome in bacteremic neonates. Compared with neonates who had three or fewer positive intravascular catheter blood cultures for coagulase-negative staphylococci, neonates who had four consecutive positive blood cultures were at significantly increased risk for end-organ damage and death. In neonates with central venous catheterassociated infection, prompt removal of the device is advised unless there is rapid clinical improvement and sterilization of blood cultures after initiation of therapy. Meningitis caused by gram-negative enteric bacilli can pose special management problems. Eradication of the pathogen often is delayed, and serious complications can occur. Mortality and morbidity were not significantly different in infants who received parenteral drug alone or parenteral plus intrathecal therapy. Cefotaxime has superior in vitro and in vivo bactericidal activity against many microorganisms. Enterococci and antibiotic-resistant, gram-negative enteric bacilli are potential pathogens in these settings. A combination of vancomycin, an aminoglycoside, and cefotaxime may be appropriate. Ceftazidime or meropenem in addition to an aminoglycoside should be considered for P. Other antibiotics may be necessary for the treatment of highly resistant organisms. Meropenem,654 ciprofloxacin,655-657 or trimethoprim-sulfamethoxazole658,659 can be the only antimicrobial agents active in vitro against bacteria that are highly resistant to broad-spectrum -lactam antibiotics or aminoglycosides. Some of these drugs require careful monitoring because of toxicity to the newborn (see Chapter 37), and ciprofloxacin has not been approved for use in the United States in infants younger than 3 months. Definitive treatment of meningitis caused by gram-negative enteric bacilli should be determined by in vitro susceptibility tests, and assistance from an infectious diseases specialist can be helpful. Use of dexamethasone as adjunctive treatment in childhood bacterial meningitis has been recommended based on reduction of neurologic sequelae in infants and children, in particular hearing loss, and especially in cases of H. Only one randomized controlled study exists for neonates, conducted in 52 full-term neonates, and the mortality (22% dexamethasone vs. Treatable diseases, such as partially treated bacterial disease, meningoencephalitis caused by herpes simplex virus, syphilis, cytomegalovirus, toxoplasmosis, Lyme disease in regions where Borrelia is prevalent, tuberculosis, and malignancy, need to be considered in the differential diagnosis. The history of illness and contacts in the mother and family and epidemiologic features, such as animal exposures and recent travel, should be explored. Reexamination of the infant for focal signs of disease, including special techniques such as ophthalmologic examination, and consideration of appropriate diagnostic imaging studies of the long bones, skull, and brain can provide further information in determining the source of infection. The introduction of sulfonamides and penicillin and later introduction of broad-spectrum antibiotics, such as chloramphenicol and streptomycin, decreased the mortality rate to about 60%. The introduction of the aminoglycosides, first with kanamycin in the early 1960s and gentamicin late in that decade, vastly improved therapy for bacteremia caused by gramnegative organisms, the leading cause of sepsis at that time. Mortality rates for sepsis, including infants of all weights and gestational ages, decreased from 40% to 50% in the 1960s4,6,286,670 to 10% to 20% in the 1970s and 1980s. Fulminant sepsis, with signs of illness present at birth or during the first day of life, has a high mortality rate, varying from 14% to 20%6,12,261,288 to as high as 70%. Clostridium, Peptococcus, and Peptostreptococcus are highly sensitive to penicillin G, but B. If anaerobic organisms are known or suspected to be responsible for infection (as in peritonitis), initiating therapy with a clinically appropriate agent, such as clindamycin, metronidazole, meropenem, ticarcillin, or piperacillin/tazobactam, is warranted. Mortality from sepsis is higher for preterm than for term infants in virtually all published studies§ but is approximately the same for all major bacterial pathogens10,260 (see Tables 6-4 and 6-5). In recent surveys, the mortality rate for neonatal meningitis has declined from 25%10,25,672,673 to 10% to 15%. Of the 38 survivors who were available for evaluation at 3 years of age or older, 29% had severe neurologic sequelae, 21% had minor deficits, and 50% were functioning normally. A comparable study evaluating 35 newborns over a period of 3 to 18 years demonstrated more favorable outcomes, with 60% of survivors considered normal at the time of follow-up compared with sibling controls, 15% with mildto-moderate neurologic residua, and 25% with major sequelae.
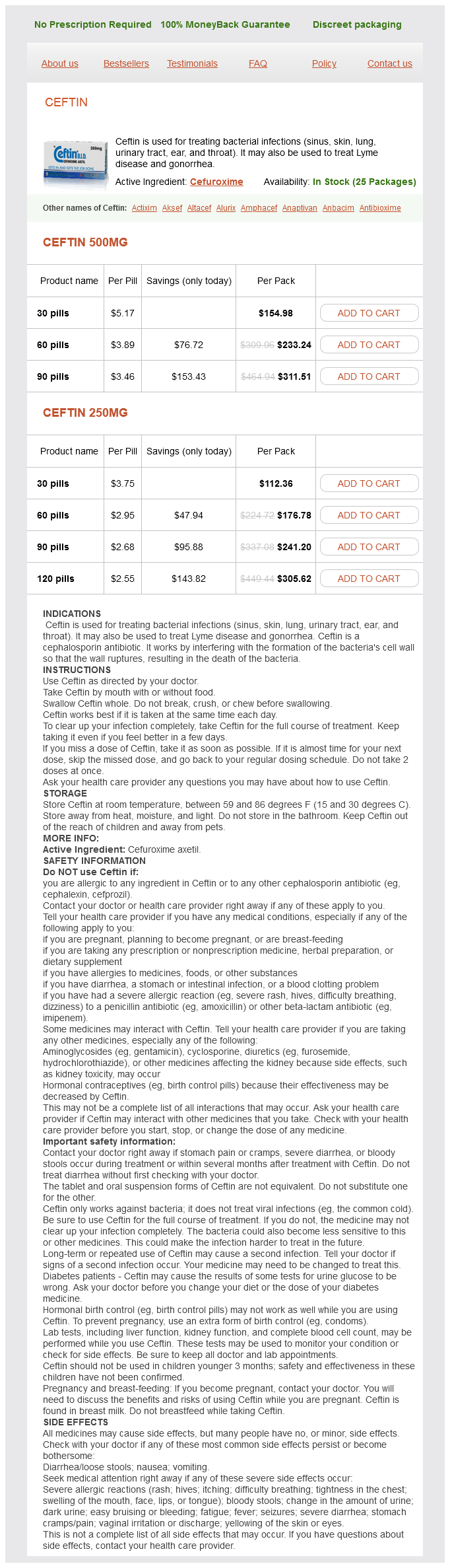
Cefuroxime Dosage and Price
Ceftin 500mg
- 30 pills - $154.98
- 60 pills - $233.24
- 90 pills - $311.51
Ceftin 250mg
- 30 pills - $112.36
- 60 pills - $176.78
- 90 pills - $241.20
- 120 pills - $305.62
Because sulfadoxine has a much longer half-life than sulfadiazine medications harmful to kidneys order cefuroxime 250 mg visa, this combination is typically administered orally every 10 days for 1 year at doses of 1. Outside of the United States, Fansidar is available as syrup, which simplifies administration. In our experience, this regimen is well tolerated and seldom leads to relevant neutropenia405; regular hematologic testing is nevertheless needed as with the standard pyrimethamine/sulfadiazine treatment regimen (see later). In a small cohort study, Fansidar has also been used to treat pregnant women in whom fetal infection was confirmed using a dosage of 25 mg of pyrimethamine and 500 mg of sulfadoxine per 20 kg of body weight and 50 mg of folinic acid on a twice-monthly basis. Under steady-state conditions, the ratio of fetal-to-maternal drug concentrations in umbilical vein blood at the time of delivery ranged from 0. After birth, the combination was continued, with the dose adjusted to the weight of the infant. In any case, and despite the lack of evidence from randomized controlled trials, the body of evidence from large 31 · Toxoplasmosis 973 nonrandomized case series indicates that the combination of pyrimethamine with sulfadiazine or sulfadoxine is beneficial, based on differences in the incidences of sequelae between treated and untreated individuals. Because pyrimethamine inhibits the activity of dihydrofolate reductase, a precursor of folic acid, it induces, as expected, a reversible and usually gradual suppression of hematopoiesis. Neutropenia is the most severe and common side effect of treatment with pyrimethamine, although reduced platelet counts and anemia are not uncommon. When the drugs are administered at the recommended doses, their plasma concentrations usually fall within the expected therapeutic limits, and the intervention is generally well tolerated (in 86% of cases). Available data afford no evidence of teratogenicity when administered in the recommended dosage,474,475 but pyrimethamine/sulfonamides should not be given in the first 14 weeks of gestation in any case. Because the toxic effects of pyrimethamine on hematopoiesis are a consequence of the induced deficiency in folic acid, which is required for cell division, this problem can be ameliorated by the co-administration of folinic acid (leucovorin). Leucovorin calcium is usually administered three times per week at a dose of 5 to 20 mg, with which regimen the inhibitory action of pyrimethamine on the proliferation of T. In rare cases, the latter can lead to severe or even fatal allergic dermatitis (Stevens-Johnson and Luell syndromes). During this phase, spiramycin can clear the parasite from the blood and reduce the frequency of placental infection. The infectious load of the placenta is also reduced, although, to attain this effect, a longer treatment duration is necessary than is required with a pyrimethamine/sulfonamide regimen. Under in vivo and in vitro conditions, spiramycin exerts an antitoxoplasmic effect, which appears to be clinically useful in preventing congenital infection with T. However, because spiramycin is not parasiticidal, its use is not recommended for the treatment of fetal toxoplasmosis. However, inhibitory concentrations are barely attained in fetal tissues and not at all in the brain. There exists no evidence that prenatal treatment with spiramycin reduces the risk of developing clinical manifestations in infants who become infected despite treatment of the mother. Although spiramycin is generally well tolerated, overdosage of newborn infants can induce potentially severe side effects. Doses greater than 35 mg/kg of body weight can provoke local vasospasm, changes in taste perception, vertigo, dizziness, flushing of the face, tearing of the eyes, nausea, vomiting, diarrhea, and anorexia. However, available data afford no evidence that clindamycin, either alone or together with other drugs, is equally or more efficacious than established systemic combination therapies for the treatment of congenital infection in either pregnant women or their newborn offspring. Atovaquone has been shown to potently inhibit the replication of both tachyzoites and bradyzoites in vitro and to reduce the fatality rate in a murine model of toxoplasmosis in a strain-dependent manner. Trimethoprim and cotrimoxazole were also effective against the parasite but at higher concentrations than those observed for artesunate and pyrimethamine. If a similar effect of artesunate could be demonstrated in vivo, without eliciting deleterious side effects, this agent could find a role in the treatment of toxoplasmosis. In contrast to sulfonamides, artemisinin and its semisynthetic derivatives artesunate, artemether, and dihydroartemisinin, are short-acting antimalarial agents that destroy the parasites more rapidly than conventional ones. However, none of these agents have been clinically tested in the context of congenital toxoplasmosis, nor, indeed, even been investigated in a murine model of toxoplasmosis. As yet, genetic resistance has not been observed with drugs used to treat infection with T. Although cotrimoxazole has been used in combination with spiramycin to treat pregnancy-associated toxoplasmosis and was well tolerated by the patients, this agent cannot be recommended on the basis of the available data. In this model, the drug averted the fatal consequences of acute infection in, and eradicated the parasite from, the livers, spleens, and brains of approximately 30% to 50% of acutely surviving animals. During the acute phase of infection in mice, clindamycin effectively inhibited the vertical transmission of the parasite from the mother to the fetus. A weekly intravitreal injection of this drug, together with dexamethasone, over a 4-week period, proved to be as effective as the recommended oral therapy with pyrimethamine and sulfadiazine in terms of the primary outcome and the prevention of recurrences over a 2-year follow-up course. Two are involved in motility and host cell invasion (the calcium-dependent protein kinase 1 and the cyclic guanosine monophosphatedependent protein kinase), two in stage interconversion (the mitogen-activated protein kinase 1 and the cyclic adenosine monophosphatedependent protein kinase), and two in cell-cycle control (the casein kinase 1 and the cdc2 cyclin-dependent kinase) cell. Because the rhoptry kinases differ greatly from mammalian protein kinase in structure and function, they would be ideal drug targets. A plant-type redox apparatus, consisting of ferredoxin nicotinamide adenine dinucleotide phosphate+ reductase and its redox partner ferredoxin, as well as lipoic acid synthase and enzymes of the isoprenoid biosynthetic pathway, could also serve as drug targets because both systems are implicated in metabolic processes that are vital for the parasite. However, as yet, studies with these drugs have been conducted exclusively under experimental conditions and have not been pursued to the stage of preclinical development and clinical evaluation. The most recent figures were estimated from a nationwide survey of subjects sampled between 1999 and 2004 and indicated that the overall age-adjusted seroprevalence of T.
© 2025 Adrive Pharma, All Rights Reserved..