General Information about Caverta
In conclusion, Caverta is a pill used to deal with ED in males. It works by rising blood flow to the penis, permitting for an erection to happen and be maintained. It is available in varied strengths and taken orally about half-hour before sexual exercise. While it's typically secure and well-tolerated, it's essential to consult with a physician earlier than utilizing Caverta to guarantee that it is appropriate for you. With its effectiveness and adaptability, Caverta has become a well-liked choice for men seeking therapy for ED and the flexibility to enjoy a fulfilling sex life as quickly as once more.
One of the principle advantages of Caverta is its effectiveness in treating ED. Studies have shown that it's highly efficient in improving erectile perform and sexual satisfaction in men with ED. It has additionally been proven to be safe and well-tolerated by most males. Additionally, Caverta could be taken on an as-needed foundation, permitting for flexibility in sexual activity.
Caverta is a medicine that has been gaining recognition among men who expertise erectile dysfunction (ED). This situation, which is usually known as impotence, is the inability to achieve or maintain an erection adequate for sexual activity. ED can be caused by a variety of components, including bodily, emotional, and psychological issues. Caverta helps to alleviate this problem by increasing blood flow to the penis, allowing men to achieve and maintain an erection.
Caverta is a tablet that accommodates sildenafil citrate, the identical energetic ingredient found within the well-known medication Viagra. Sildenafil citrate works by blocking the motion of an enzyme called phosphodiesterase kind 5 (PDE-5), which is answerable for breaking down a chemical in the body generally identified as cyclic guanosine monophosphate (cGMP). cGMP is answerable for stress-free the smooth muscular tissues in the blood vessels that offer the penis, permitting for elevated blood move. By inhibiting PDE-5, sildenafil citrate helps maintain an erection by keeping cGMP ranges high.
Caverta is out there in various strengths, including 25mg, 50mg, and 100mg. The really helpful starting dose is 50mg, but your physician could adjust the dose primarily based in your response and tolerability. It is normally taken orally, about half-hour to 1 hour before sexual exercise. The effects of Caverta can last up to 4 hours, providing an sufficient window for sexual exercise.
Caverta is a prescription-only medication, and it's essential to consult together with your doctor earlier than using it. Your physician will assess your medical history and any present medicines you take to make sure that Caverta is safe for you. It is especially essential to inform your physician in case you have any underlying well being situations, such as heart illness, hypertension, or liver or kidney problems. Also, remember to inform your physician if you're taking any medications that may work together with Caverta, such as nitrates or alpha-blockers.
It is important to notice that Caverta is not an aphrodisiac and gained't work with out sexual stimulation. It can be not a treatment for ED, but rather a treatment that helps males with this situation to take pleasure in a wholesome sexual life. Like any treatment, Caverta could trigger unwanted facet effects, but they are usually delicate and temporary. These may embody headache, dizziness, flushing, upset stomach, and nasal congestion. In uncommon cases, Caverta may trigger extra extreme unwanted effects such as vision adjustments, hearing loss, and priapism (an erection lasting more than four hours). If you expertise any of those severe side effects, search medical consideration immediately.
Methotrexate erectile dysfunction drugs walmart 100 mg caverta purchase with mastercard, sulfasalazine, and hydroxychloroquine were tapered without evidence of recurrent disease. Five patients were given infliximab (4 received 5 mg/kg and 1 received 3 mg/kg), 4 etanercept (50 mg/week), and 1 adalimumab (40 mg every 2 weeks). Nine of 10 patients had improvement in their rheumatic symptoms with a median of 15 days for >30% improvement in their pain score and tender joint count, and a median of 33 days for >30% improvement in their swollen joint count. Improvement of anterior uveitis (in 5 patients after 6 months) and cutaneous manifestations were also noted. Spectacular evolution of reactive arthritis after early treatment with infliximab Thomas-Pohl M, Tissot A, Banal F, Lechevalier D. A case report describing a 32-year-old male with acute febrile polyarthritis 1 month after gastrointestinal infection. Immediately after the infusion, he reported a decrease in pain with improvement of inflammatory markers. The authors also report substantial heterogeneity in the results and attributed this to differences in study design. A prospective randomized trial with 42 patients who had evidence of chronic postchlamydial reactive arthritis. Patients were randomized to receive either doxycycline and rifampin (12 patients), azithromycin and rifampin (15 patients), or matching oral placebos (15 patients) for 6 months; 22% of subjects on combination antibiotic therapy achieved complete resolution of their symptoms in comparison to 0% of those receiving placebo. It typically begins after trauma, such as a fracture, soft tissue injury, or surgery, and the associated pain is usually disproportionate to the expected course of injury. In addition to pain, if untreated, patients will suffer from swelling, limited range of motion, patchy bone demineralization, and skin changes. Acutely, it begins with throbbing or burning pain and is associated with localized edema. Stage two begins 2435 a few months later, when the disease progresses to soft tissue damage, and is characterized by brawny, thickened skin and muscle wasting. Finally, the third, or atrophic, phase involves ridged nails, atrophic skin changes, and limitations of movement. Early diagnosis, however, can be quite challenging as the localized edema is often mistaken for other skin conditions. As a result, dermatologists can play a crucial role in its diagnosis and management. Symptoms tend to affect a distal limb, and the patient will describe a history of trauma. The majority of patients will complain of impairment in motor function, which may involve paresis and clumsiness. About 70% of patients will describe hypoesthesia, most frequently in a stockinglike or glovelike distribution. Other dysesthetic symptoms include allodynia (pain to touch), hyperpathia (exaggerated response to painful stimuli), and anesthesia dolorosa, when an area has lost its sensitivity to touch but demonstrates severe pain. Physical examination findings, particularly in the earlier stages, include edema, which is secondary to autonomic dysfunction. Atrophy and skin discoloration can occur during the later phases, along with atrophy of the soft tissues, bones, and muscles. This is a result of a variety of skin and connective tissue changes, including increased hair growth, changes in nail growth, skin atrophy, and contraction and fibrosis of joints and fascia. First, the patient must have continuing pain that is disproportionate to the inciting event. The patient must also have at least one sign in two or more of the categories, as well as report at 2436 least one symptom in three or more of the categories. The differential diagnoses include infection, compartment syndrome, peripheral vascular disease, peripheral neuropathy, rheumatoid arthritis, deep vein thrombosis, Raynaud phenomenon, vascular thoracic outlet syndrome, conversion disorder, and factitious disorder. Based on the presenting symptoms, it is reasonable to suspect an inflammatory arthropathy or vasculitis. The efficacies of a pain 2437 management specialist are largely unknown, although referral is a reasonable option. Second-line treatment involves interventional therapies, including sympathetic nerve blockade and spinal cord stimulation. Early interventional nerve blocks may help reduce pain, allowing patients to complete more rigorous physical therapy and therefore allowing for more rapid improvement. They can also help to objectively identify abnormal characteristics of the disease. Plain radiography can monitor significant changes over time, especially if normal at baseline. Patchy osteoporosis and periarticular osteopenia is often seen in plain radiographs as early as 2 weeks after onset of symptoms. Bone scans are extremely sensitive, although nonspecific, and can often detect osseous changes before plain radiography. As disease duration progresses, studies have shown the sensitivity of bone scans decreases, whereas specificity increases. Densitometry will often reveal lowered bone mineral density early in the disease course, but as therapy progresses, density should improve. Thermography can be helpful in the diagnostic phase and allows the measurement of several symmetric points on the affected and contralateral extremity.
Treatment is usually only indicated if there is secondary bacterial infection or immunosuppression erectile dysfunction doctor new orleans buy caverta without a prescription. Preventive measures include vaccination of sheep before the lambing period to boost immune response and the wearing of gloves, if possible, when handling animals with any sign of the disease. Idoxuridine, surgery, and cryotherapy have been suggested to reduce the time to healing. For immunosuppressed individuals, infection with orf may result in a more persistent or progressive infection or giant orf. In such cases, interventional treatment is warranted, and often treatments can be combined. Idoxuridine, cryotherapy, cidofovir, interferon, and topical imiquimod cream have been reported to show benefit. Detailed description of clinical and histologic features of 19 cases of orf infection. Method for molecular diagnosis of orf initially used as research tool but now used in the United States. He was treated successfully with debulking surgery followed by repeated cryotherapy and imiquimod for a total of 17 weeks. The orf lesion of a healthy female was treated with 40% idoxuridine in dimethyl sulfoxide three times daily for 6 days. After 40% idoxuridine topically, further surgery, and repeated cryotherapy, the lesion resolved. A large palmar orf lesion was excised and small local recurrences treated with 40% idoxuridine. A case of human orf in an immunocompromised patient treated successfully with cidofovir cream Geerinck K, Lukito G, Snoeck R, DeVos R, DeClercq E, Vanrenterghem Y, et al. An immunosuppressed renal transplant patient developed a persistent giant orf lesion. Treatment with 1% cidofovir cream daily for five cycles of 5 days of treatment alternating with 5 rest days plus debridement as necessary led to full resolution of the lesion. A tumorlike orf lesion in an immunosuppressed patient was unresponsive to surgery and idoxuridine. Rapid improvement of human orf (ecthyma contagiosum) with topical imiquimod cream; report of four complicated cases Erbaci Z, Erbaci I, Almila Tuncel A. Treatment with imiquimod 5% applied twice daily for up to 10 days to orf lesions complicated by erythema multiforme, angioedema, or as giant orf possibly hastened clearance of the orf lesion and the secondary effects. Giant and multifocal orf in a patient with non-Hodgkin lymphoma did not respond to debulking and topical cidofovir. Imiquimod 5% cream applied on alternate days led to improvement after a week and clearance within 2 months. It is important when making a diagnosis to establish its morphology and the presence of any associated ectodermal disease at sites other than the palms and soles. Hyperkeratosis of the palms and soles can also be a feature of eczema, psoriasis, and cutaneous T-cell lymphoma. Most therapeutic options produce only short-term improvement and are frequently complicated by unwanted adverse effects. Treatment options range from simple measures such as saltwater soaks with physical paring of the skin and use of topical keratolytics, through to systemic retinoids and reconstructive surgery with total excision of the hyperkeratotic skin followed by grafting. In patients with limited disease, topical keratolytics containing salicylic acid, lactic acid, or urea in a suitable emollient base may be tried. Examples include 5% to 10% salicylic acid, 20% to 70% propylene glycol, or 10% lactic acid in aqueous cream or a combination therapy using 10% urea and 5% lactic acid in aqueous cream to be applied twice daily. These formulations can be made up on an individual basis or the closest proprietary product prescribed. Good responses have been seen in mal de Meleda, PapillonLefèvre syndrome, and erythrokeratoderma variabilis. The potential risk of bone toxicity should also be assessed in patients on long-term therapy, although the risks are small. Periodic radiologic bone monitoring and, when possible, prescription of pulsed (intermittent) therapy are recommended. Oral administration of 1,25-dihydroxyvitamin D3 and topical calcipotriol ointment has been reported to be effective. Regular intermittent use of terbinafine cream and other topical antifungals can reduce skin maceration and improve comfort. Surgical or laser dermabrasion is an option for some patients, with potential amelioration of symptoms and improved penetration of topical agents. Excision should remove hyperkeratotic skin, including dermis, epidermis, and subcutis, to prevent any risk of recurrence. Specific Investigations · Scrapings for mycology · Thyroid function tests An epidemiologic investigation of dermatologic fungus infections in the northernmost county of Sweden (Norbotten) 197781 Gamborg Nielson P. Hereditary palmoplantar keratoderma and dermatophytosis in the northernmost county of Sweden (Norbotten) Gamborg Nielson P. In relatives of the original case, dermatophytosis was found in 65% of men, 22% of women, and 21% of children, resulting in a total 1938 frequency of 36. Vesicular eruptions along the hyperkeratotic border occurred significantly more often in patients with dermatophytosis and were considered pathognomonic of secondary dermatophytosis. First-Line Therapies Alleviation of the plantar discomfort caused by pachyonychia congenita with topical applications of aluminum chloride and salicylic acid ointments Takayama M, Okuyama R, Sasaki Y, Ohura T, Tagami H, Aiba S.
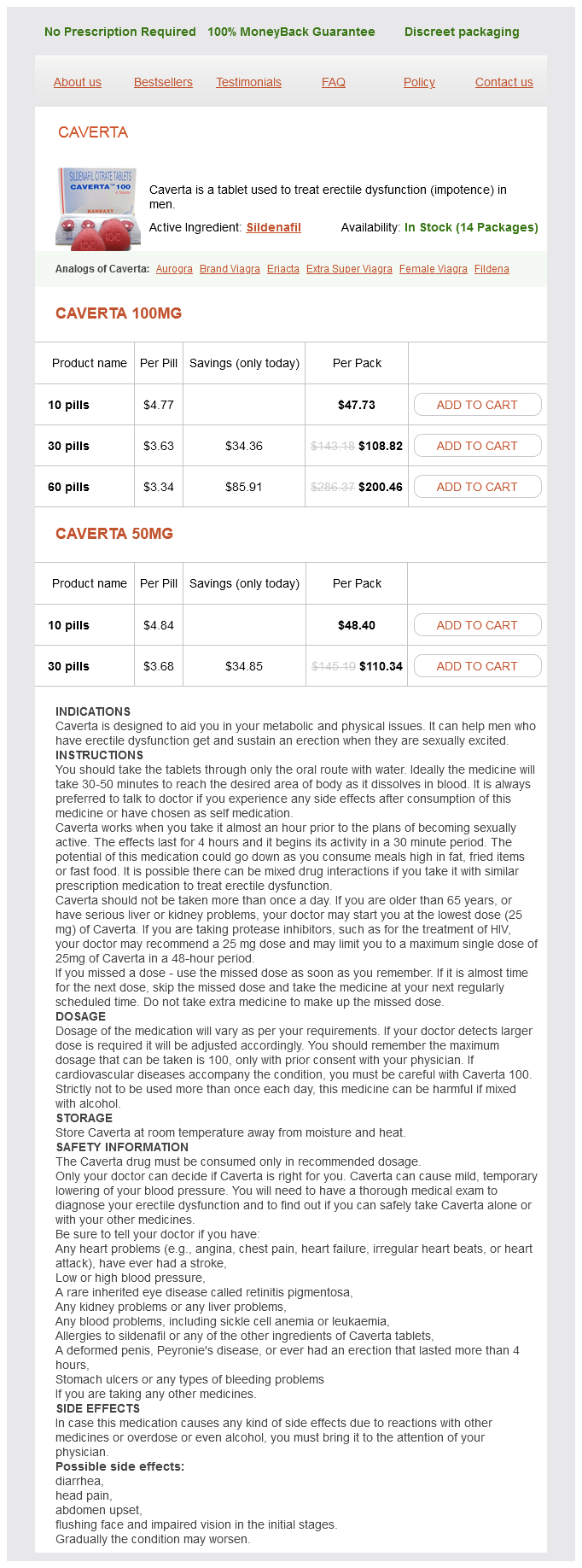
Caverta Dosage and Price
Caverta 100mg
- 10 pills - $47.73
- 30 pills - $108.82
- 60 pills - $200.46
Caverta 50mg
- 10 pills - $48.40
- 30 pills - $110.34
In a retrospective study of 80 patients treated with postoperative single-fraction radiotherapy erectile dysfunction drugs and hearing loss cheap generic caverta canada, 9% of keloids relapsed after 1 year and 16% relapsed after 5 years. Retrospective analysis of treatment of unresectable keloids with primary radiation over 25 years Malaker K, Vijayraghavan K, Hodson I, Al Yafi T. In this retrospective study involving 86 keloids in 64 patients, 97% of keloids showed significant regression after completing radiotherapy with either kilovoltage x-rays or electron beams, without significant side effects. The patients were treated with a total of 3750 cGy administered in five once-weekly fractions. Postoperative 192Ir brachytherapy showed better cosmetic results at higher dosages, with only one keloid recurrence out of 38 observed after a once-administered 6-Gy and twice-administered 4-Gy regimen. Postkeloidectomy irradiation using high-dose-rate superficial brachytherapy Kuribayashi S, Miyashita T, Ozawa Y, Iwano M, Ogawa R, Akaishi S, et al. A total of 36 keloids were treated with high-dose-rate superficial brachytherapy after keloidectomy. Systematic review of 33 articles that contained 3130 patients with 3470 keloid scars treated with excision followed by low-dose or highdose brachytherapy. High-dose brachytherapy showed lower recurrence rates compared with low-dose brachytherapy and external radiation, and a short time (<7 hours) interval postexcision was associated with lower recurrence rate compared with long time interval (>24 hours). Twelve patients with a total of 16 lobule keloids were treated with 980-nm diode laser and subsequent intralesional triamcinolone acetonide injection. Between two and five treatment sessions led to 75% of patients with more than 75% reduction of keloid size, with no recurrence in the past 12 months. In 19 patients with keloidal or hypertrophic median sternotomy scars, pulsed dye laser with pulse width of 0. One had no recurrence, 9 required corticosteroids to suppress recurrence, and 13 were considered to be treatment failures. Pilot study of the effect of postoperative imiquimod 5% cream on the recurrence rate of excised keloids Berman B, Kaufman J. Thirteen keloids were treated with excision and imiquimod 5% cream every night for 8 weeks. Ten patients with 11 keloids completed the 6-month study, and there were no recurrences. Role of mitomycin C in reducing keloid recurrence: patient series and literature review Gupta M, Narang T. Twenty patients with 26 earlobe keloids were treated with surgical shave excision and topical mitomycin C. Five of the 10 study patients had a reduction in their scar size by at least 50% in linear dimensions. There was a reduction in keloid size and symptoms in 77% of 28 intractable keloids treated with topical retinoic acid. Over 3 months, four courses of bleomycin were administered through a multiple superficial puncture technique in 50 patients with keloids and hypertrophic scars. Forty-four percent of patients experienced complete flattening of lesions, and 22% showed more than 75% lesion regression. In this randomized, single-blind, parallel group study in which 54 patients were allocated to receive either verapamil (2. Triamcinolone had a faster reduction rate, but verapamil had a lower rate of hypopigmentation. Typically, the 1363 lesion presents as a rapidly growing (weeks to months) crateriform nodule on sun-exposed skin of the middle aged or elderly Caucasian. During the proliferative phase, lesions grow quickly and can reach an impressive size. Histologically, for example, lesions appear as a symmetric exoendophytic proliferation of glassy keratinocytes with a central keratin-filled crater. Once a diagnosis has been established, management aims to stimulate resolution, prevent local destruction, minimize the risk of recurrence, and achieve a favorable cosmetic outcome. Low-risk lesions in select candidates may be treated with destructive methods such as cryotherapy or electrodesiccation and curettage. If confidence in a diagnosis can be ascertained, observation can be entertained, but with great caution. Large lesions may be treated with topical (imiquimod or 5-fluorouracil) or intralesional (5-fluorouracil, methotrexate, or bleomycin) chemotherapy or x-ray therapy. For locally recurrent lesions, Mohs micrographic surgery reduced the rate of recurrence from 23. The author reports his experience using cryosurgery to a temperature of -50° to -60°C for 4406 new and recurrent skin cancers in 2932 patients. Natural course of keratoacanthoma and related lesions after partial biopsy: clinical analysis of sixty-six tumors Takai T, Misago N, Murato Y. Intralesional methotrexate treatment for keratoacanthoma 1367 tumors: a retrospective case series Aubut N, Alain J, Claveau J. Complete remission was noted in all reported cases within 4 to 11 weeks; application frequencies ranged from twice daily to three times weekly. Two patients experienced temporary erythema, and all reported satisfaction with the treatment. No evidence of recurrence was noted, and excellent cosmetic outcomes were reported at 3 years of follow-up. Multiple keratoacanthomas First-Line Therapies 1369 Acitretin induces remission in generalized eruptive keratoacanthoma of Grzybowski Sami N, Bussian A. After 6 months of acitretin 25 mg/d, all initial lesions resolved and no new lesions developed.
© 2025 Adrive Pharma, All Rights Reserved..