General Information about Cardura
The primary operate of Cardura is to chill out and widen the blood vessels, which in turn lowers blood pressure and allows blood to flow extra simply through the body. This lowers the risk of heart assaults, strokes, and different cardiovascular problems. In addition, Cardura additionally works to enhance urinary signs in men with BPH by stress-free the muscular tissues within the prostate and bladder, making it simpler to urinate.
In conclusion, Cardura is a highly effective medicine for managing hypertension and urinary signs in men with BPH. It has been used for many years and has confirmed to be secure and well-tolerated by most patients. However, it is necessary to comply with the really helpful dosage and to tell your physician of any unwanted effects or interactions with different medications. With correct use and monitoring, Cardura can help improve the standard of life for those dwelling with hypertension or BPH.
Cardura, also known by its generic name doxazosin, is a medication that's generally used for 2 major purposes: treating hypertension and managing symptoms of benign prostatic hyperplasia (BPH). This powerful drug belongs to a class of medicines generally identified as alpha blockers, and has been proven to be an effective remedy choice for patients suffering from these situations.
It is important to tell your doctor about any other drugs you are taking earlier than beginning Cardura. It might work together with other medication and cause doubtlessly harmful unwanted facet effects. It must also be used with caution in patients with liver or kidney disease, as well as in those with low blood stress.
BPH, however, is a non-cancerous enlargement of the prostate gland that may cause troublesome urinary signs in males. As males age, the prostate naturally grows in measurement, which might cause strain on the bladder and urethra, resulting in issue in urination and other symptoms similar to frequent urination, weak urine stream, and the sensation of incomplete bladder emptying. BPH primarily affects males over the age of 50 and might tremendously affect their high quality of life. Cardura works by relaxing the muscles within the prostate and the bladder, making it simpler for men to urinate.
High blood strain, also referred to as hypertension, is a typical condition that impacts tens of millions of people worldwide. It is sometimes called a silent killer as a outcome of it often has no warning indicators or symptoms until severe problems come up. If left uncontrolled, high blood pressure can result in serious well being issues such as heart disease, stroke, and kidney failure. Cardura helps to lower and keep a wholesome blood stress stage, thereby reducing the chance of those harmful circumstances.
Cardura comes in the form of oral tablets and is normally taken as quickly as a day with or without food. The dose may be adjusted by a healthcare supplier based on the individual's response to the treatment. It is important to take Cardura at the same time daily to maintain up a steady level of the drug within the body. It might take a number of weeks for the medication to show its full results, so it's important to not stop taking it with out consulting a doctor.
Like any treatment, Cardura could cause some side effects, although not everybody experiences them. Common unwanted facet effects embrace dizziness, lightheadedness, nausea, and headaches. These often subside as the physique adjusts to the treatment. In some instances, severe side effects corresponding to fainting, difficulty respiration, and chest pain could happen, and quick medical attention should be sought if these happen.
Blue nevus this is a collective term for several types of nevi whose principal common pathological criterion is the proliferation of spindle-shaped and dendritic melanocytes in the dermis blood pressure medication and lemon juice cheap cardura 4 mg buy on-line. The most important of these are the so-called common blue nevus and the cellular blue nevus. Because these dermatopathological sub-groups cannot be identified clinically or by dermatoscopy, when we only show the clinical or dermatoscopic appearance, we use the collective term "blue nevus". If the nevus was excised and subjected to histological investigation (which occurred in most cases), the dermatopathological sub-classification is also given. Clark nevus the Clark nevus is the most common type of acquired melanocytic neoplasm. They are usually macular, ranging in size from a few millimeters up to about 1 cm. Occasionally, but more commonly in persons with a © Dies ist urheberrechtlich geschütztes Material. Middle row, left: this patient has several Clark nevi as well as numerous "small" congenital nevi, of which the majority are larger than the Clark nevi. In some cases it may not be possible to distinguish between a Clark nevus and a congenital nevus with the naked eye. Middle row, right: A typical Clark nevus (arrow), surrounded by other nevi which cannot be definitely classified on clinical investigation (Clark nevus or "superficial" congenital nevus). Clark nevi usually occur on the trunk and the proximal portion of the extremities, but not on facial or acral skin. On average, people with lighter skin phototypes have ten to twenty, but it is not unusual to see people with hundreds of Clark nevi. In terms of dermatopathology Clark nevi have a characteristic appearance: the silhouette is symmetrical and flat, and the melanocytes are located in small, regular nests at the dermo-epidermal junction (junctional Clark nevus). Occasionally one finds small nests of melanocytes in the papillary dermis as well (compound type of Clark nevus). In contrast to the "superficial" congenital nevus, these nests do not entirely fill the papillary dermis. He considered this nevus an intermediate step in the development of melanoma and therefore called them "dysplastic nevi". Unfortunately Clark incorporated several different types of nevi in the term, with many of the nevi termed "dysplastic" by Clark actually being "superficial" or "superficial and deep" congenital nevi (2. Many histopathologists continue to use the term "dysplastic" and continue to include various small congenital nevi under this name. Clark nevi may mimic melanoma and therefore occasionally require excision for diagnostic reasons. Prophylactic excision is not indicated because the risk of malignant transformation of a single Clark nevus is extremely low. The majority of melanomas arise de novo; they do not arise from a pre-existing nevus. Congenital nevus In the absence of further specification this is an ambiguous collective term used to mean different things by clinicians and pathologists. Clinicians refer to melanocytic nevi as congenital only when they are visible during or shortly after birth or when the size of the nevus does not permit any other differential diagnosis. Depending on their size, these nevi are sub-divided into large (> 20 cm), medium-sized (1. At the end of their period of growth, congenital nevi are usually raised above the skin and may be heavily or lightly pigmented. The size of a congenital nevus is proportional to the likelihood of the nevus being visible at birth. When dermatopathologists refer to a congenital nevus they are usually talking about a nevus with a specific type of fine tissue architecture (arrangement and distribution of melanocytes), which obviously remains invisible to the clinician. Whether the nevus was present at birth or not, as well as its size, are of little importance to the dermatopathologist. The two types of congenital nevus are the "superficial" congenital nevus (Ackerman nevus) in which the accumulation of melanocytes is no deeper than the papillary dermis, and the "superficial and deep" congenital nevus (Zitelli nevus) in which melanocytes extend at least into the reticular dermis. Many of the nevi termed "dysplastic" or "atypical" in patients with so-called "dysplastic nevus syndrome" are actually small congenital nevi (2. These patients are subject to a higher risk of melanoma because the number of congenital nevi is very likely an expression of a genetic predisposition. As mentioned earlier, many dermatologists and dermatopathologists adhere to a different concept and refer to Clark nevi as well as "superficial" and "superficial and deep" congenital nevi as "dysplastic nevi". This creates the wrong impression that one is referring to the same type of nevus. The nevi numbered 1 and 2 have excess terminal hair, clearly indicating their congenital nature. These patients are diagnosed with a "dysplastic" or "atypical nevus syndrome", although some nevi such as those shown here are quite obviously congenital. Adjacent to it (E, F) are corresponding photographs of a "superficial and deep" congenital nevus (Zitelli nevus). In Clark nevi (C, D) there are small nests of melanocytes at the dermo-epidermal junction (arrows in image D) while the papillary dermis is largely unaffected (the cells in the papillary dermis are inflammatory cells and melanophages). The "superficial and deep" congenital nevus (G, H) has a different histopathological appearance. The melanocyte nests are large and are present in the papillary (therefore superficial) as well as the reticular dermis (therefore deep). In a Clark nevus as we define it, nests of melanocytes are found no deeper than the papillary dermis.
Femoral neck fractures are commonly treated with hemiarthroplasty or total hip replacement arteria lusoria definition cardura 4 mg buy with amex. Peritrochanteric hip fractures are treated with open reduction internal fixation, where plate and screw construct or intramedullary devices are used. Since fracture fixation requires the fracture to proceed to union, the patient may need to have protected weight bearing during the early postoperative period. Dislocation, periprosthetic fracture, and avascular necrosis of the hip are common complications after surgery. The surgical trends for treating femoral neck fractures show a rise in use of arthroplasty, which was possibly reflecting a rising trend toward specialty care (more arthroplasty surgeon care). Patients should be mobilized as soon as possible postoperatively to avoid pulmonary complications and pressure injuries (formerly pressure ulcers). Supervised physical therapy and rehabilitation are important for the patient to » Treatment s errs ook e ook e/eb e/eb /t. Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Changing trends in the treatment of femoral neck fractures: a review of the American Board of Orthopaedic Surgery database. Dedicated perioperative hip fracture comanagement programs are cost-effective in high-volume centers: an economic analysis. Mechanical symptoms-such as swelling, grinding, catching, and locking-suggest internal derangement, which is indicated by damaged cartilage or bone fragments that affect the smooth range of motion expected at an articular joint. Patients complain of pain deep in the groin on the affected side and have problems with weight-bearing activities such as walking, climbing stairs, and getting up from a chair. They may limp and develop a lurch during their gait, leaning toward the unaffected side as they walk to reduce pressure on the hip. Minimally invasive surgeries and computer-assisted navigation during operation are being investigated as methods to improve techniques (eg, accurate placement of the hardware implant) and to reduce complication rates. Rather than use a traditional artificial joint implant of the whole neck and femur, only the femoral head is removed and replaced. Evidence to date suggests that hip resurfacing is comparable to total hip replacement and is a viable alternative for younger patients. Concerns following resurfacing surgery include the risk of femoral neck fracture and collapse of the head. Dislocations were more frequent with total hip arthroplasty than metal-on-metal hip resurfacing: 4. Guidelines recommend prophylaxis for venous thromboembolic disease for a minimum of 14 days after arthroplasty of the hip or knee using warfarin, lowmolecular-weight heparin, fondaparinux, aspirin, rivaroxaban, dabigatran, apixaban, or portable mechanical compression (see Table 1414). Effect of physical therapy on pain and function in patients with hip osteoarthritis: a randomized clinical trial. Association of hip pain with radiographic evidence of hip osteoarthritis: diagnostic test study. Prevention of venous thromboembolic disease after total hip and knee arthroplasty. Hip resurfacing versus total hip arthroplasty: a systematic review comparing standardized outcomes. Arthroscopic versus open treatment of femoroacetabular impingement: a systematic review of medium- to long-term outcomes. Acute knee swelling (due to hemarthrosis) within 2 hours may indicate ligament injuries or patellar dislocation or fracture. Lateral "snapping" with flexion and extension of the knee may indicate inflammation of the iliotibial band. Pain that occurs when rising after prolonged sitting suggests a problem with tracking of the patella. A careful history coupled with a physical examination that includes observation, palpation, and range of motion testing, as well as specific tests for particular anatomic structures is frequently sufficient to establish a diagnosis. When there is a knee joint effusion caused by increased fluid in the intra-articular space, physical examination will demonstrate swelling in the hollow or dimple around the patella and distention of the suprapatellar space. Table 415 shows the differential diagnosis of knee pain, and Table 416 outlines possible diagnoses based on the location of pain. Separating and cushioning these bony surfaces is the lateral and medial meniscal cartilage, which functions as a shock absorber during weight bearing, protecting the articular cartilage. It is embedded in the quadriceps tendon, and it articulates with the trochlear groove of the femur. Poor patellar tracking in the trochlear groove is a common source of knee pain especially when the cause is atraumatic in nature. The knee is stabilized by the collateral ligaments against varus (lateral collateral ligament) and valgus (medial collateral ligament) stresses. They act to decrease friction of tendons and muscles as they move over adjacent bony structures. Excessive external pressure or friction can lead to swelling and pain of the bursae. The prepatellar bursae (located between the skin and patella), and the pes anserine bursa (which is medial and inferior to the patella, just below the tibial plateau) are most commonly affected. Joint fluid, when excessive due to synovitis or trauma, can track posteriorly through a potential space, resulting in a popliteal cyst (also called a Baker cyst).
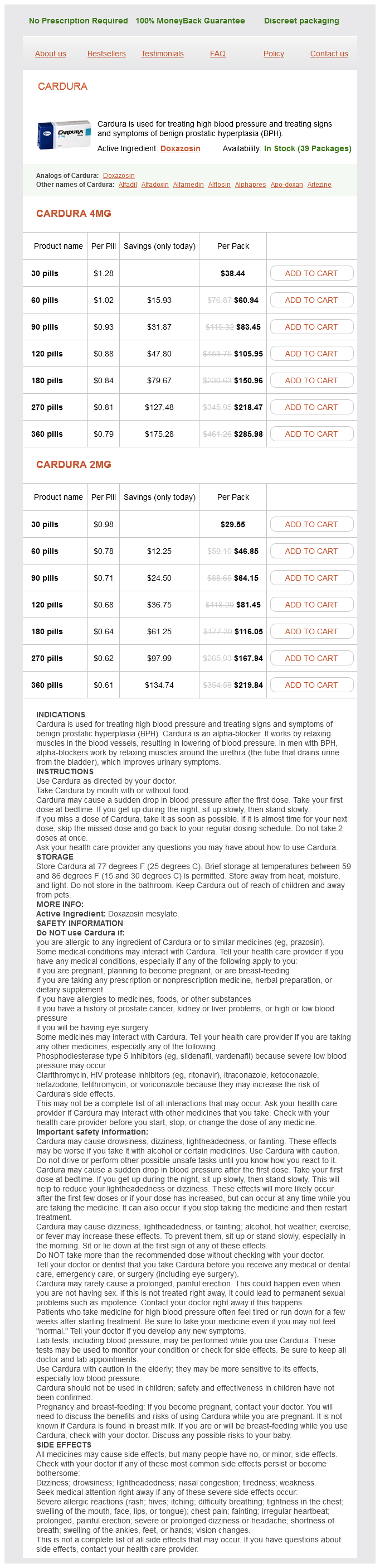
Cardura Dosage and Price
Cardura 4mg
- 30 pills - $38.44
- 60 pills - $60.94
- 90 pills - $83.45
- 120 pills - $105.95
- 180 pills - $150.96
- 270 pills - $218.47
- 360 pills - $285.98
Cardura 2mg
- 30 pills - $29.55
- 60 pills - $46.85
- 90 pills - $64.15
- 120 pills - $81.45
- 180 pills - $116.05
- 270 pills - $167.94
- 360 pills - $219.84
Medications administered by the oral route of administration may be subject to first-pass metabolism by hepatic enzymes prehypertension hypothyroidism cheap cardura 4 mg online, reducing the amount of administered drug that reaches the systemic circulation. Fentanyl is now available as several transmucosal formulations intended for sublingual, buccal, or intranasal administration. Highly concentrated oral opioid solutions are frequently instilled in the buccal or sublingual cavity. A small, but variable portion of the oral solution is actually absorbed transmucosally, but the portion that gets absorbed through the mucosal membranes in the mouth bypasses the liver; therefore, it is not subject to a first-pass effect. The variability in transmucosal absorption reflects the lipophilicity of the opioid. Buprenorphine, fentanyl, and methadone are more lipophilic, and a larger percentage of the transmucosally administered dose is absorbed directly from the site of administration. Transmucosally absorbed opioids have a rapid onset of action due to the good blood supply to the area of absorption. The rest of the medication is swallowed and absorbed, subject to the first-pass effect. Disadvantages to buccal and sublingual opioid administration include the inconvenience of holding the dosage formulation in the mouth and the relatively poor transmucosal absorption of morphine and oxycodone. Rapid-acting fentanyl products will be discussed in detail in Chapter 4, and they have a much higher degree of transmucosal absorption than morphine or oxycodone solution. Opioid suppositories inserted just past the rectal sphincter avoid first-pass hepatic metabolism, although suppositories inserted higher into the rectal vault are absorbed into the superior rectal vein that empties into the hepatic circulation, resulting in first-pass metabolism. Morphine rectal suppositories are approximately bioequivalent to oral morphine (1:1 dosing conversion), and are usually dosed every 4 hours. Rectal methadone is not commercially available; however, evidence shows it is approximately bioequivalent to oral methadone. Generally, practitioners use a 1:1 ratio for oral:controlledrelease morphine tablets administered rectally, although the rectal dose may require dosage reduction due to increased sedation from better absorption. For example, if 30 mg of oral morphine were administered by mouth, and 10 mg of the drug was absorbed unchanged, the bioavailability would be 1/3, or 33%. You learned how the first-pass effect can dramatically affect bioavailability, as is the case with drugs such as fentanyl (metabolized to inactive metabolites by the P450 system), morphine (metabolized to active and potentially toxic metabolites via glucuronidation), lidocaine, and nitroglycerin. We can minimize this effect by giving nitroglycerin by the sublingual route, bypassing the liver prior to absorption, or administering lidocaine topically (Lidoderm topical patch) or intravenously. Medications that are either extremely water-soluble (hydrophilic) or extremely lipid-soluble (hydrophobic or lipophilic) are poorly absorbed either because they cannot cross the lipidrich cell membranes or they cannot dissolve into solution. For optimal drug absorption, the medication must be primarily lipophilic, but also be sufficiently soluble in aqueous solutions. Some medications are unstable in the pH of gastric contents, such as penicillin G. This includes factors such as drug particle size, salt form, crystal polymorphism, and the presence of various excipients. Excipient is a fancy word for all the stuff aside from the drug itself in the tablet or capsule. First, patients tend not to like this route, and it makes for uncomfortable family dynamics when a 60-year-old man has to administer a rectal suppository to his 85-year-old mother. In addition to emotional discomfort, rectal products can be physically uncomfortable for patients with advanced illnesses. Dehydrated patients may have insufficient fluid in the rectal vault to absorb medications delivered by this route. Rectal drug products should not be administered into surgically created openings, and are less helpful in patients with diarrhea, colostomy, hemorrhoids, anal fissures, or in neutropenic patients. Rectal doses can be expelled before they are fully absorbed, and, if the lower rectum is filled with stool, absorption will also be limited. This can only be proven by performing a rectal examination, and for obvious reasons, this creates an additional burden for the patient and caregiver. Drugs can be injected into a peripheral vein over several minutes, or administered by an intermittent or continuous infusion. Patients are also frequently fearful of more invasive or painful medications given by injection. Sub-Q administration of a medication involves much less equipment and may be administered by the patient or a family member. Opioids may be administered by intermittent sub-Q injections or continuous sub-Q infusion. Disadvantages to the sub-Q route of administration include potential discomfort, local tissue irritation, and probably most important, the need to limit the volume injected (because the subcutaneous tissue has a limited capacity to absorb fluid). Some references cite a maximum of 2 mL per injection, or 1 to 2 mL/hr of continuous sub-Q infusion. With high doses, however, absorption may be more variable with sub-Q injections or infusion and may require dosage adjustment. Some literature suggests that the relative potency ratio of sub-Q to oral morphine is between 1:2 and 1:3 with doses in excess of 10 mg/hr (our table states it is 1:2. Remember the steps outlined in Chapter 1, Table 1-2, that summarize the five steps in opioid conversion calculations. Table 2-2 in this chapter shows you four possible conversion calculation methods-What a deal!
© 2025 Adrive Pharma, All Rights Reserved..