General Information about Bystolic
This makes Bystolic not only an effective therapy for high blood pressure, but in addition a possible device in preventing other health issues such as heart disease and stroke. Bystolic is on the market in tablet form and is often taken once a day. It is important to take Bystolic as directed by a physician, as sudden withdrawal of the medicine can lead to a rise in blood pressure.
It is used to deal with hypertension (hypertension) and to forestall chest ache (angina). Bystolic works by blocking the results of certain pure chemicals within the body, such as adrenaline, which might increase heart price and blood stress. By slowing down the guts fee, Bystolic allows the center to work more effectively and decreases the workload on the center.
This results in a decrease in blood pressure and a reduction within the pressure on the heart, which may help forestall conditions such as coronary heart attacks and strokes. Bystolic has additionally been shown to enhance exercise tolerance in sufferers with coronary heart failure. In addition to its effects on the center, Bystolic also has helpful effects on blood vessels. It relaxes the blood vessels, which helps to improve blood flow and cut back blood pressure. This could be particularly beneficial for people who have peripheral artery illness, as it may possibly enhance blood circulate to the limbs and scale back signs of leg ache. Bystolic can additionally be distinctive in that it has antioxidant properties, which means it could defend the physique from harmful free radicals that can damage cells and tissues.
Bystolic is usually well tolerated, with common unwanted facet effects together with fatigue, dizziness, and headache. However, as with any medication, there's a danger of extra serious side effects similar to problem respiratory, chest ache, or fainting. It is important for sufferers to debate any considerations or potential unwanted facet effects with their doctor. Bystolic is a highly efficient treatment for managing hypertension and has proven to enhance overall cardiovascular health. It is an important software in the battle in opposition to coronary heart disease and must be thought of as a part of a complete remedy plan for those with hypertension.
Sporer A arrhythmia associates fairfax va cheap bystolic 5 mg, Leyson J, Martin B: Effects of bethanechol chloride on the external urethral sphincter in spinal cord injury patients, J Urol 120:6267, 1978. Staskin D, Kay G, Tannenbaum C, et al: Trospium chloride has no effect on memory testing and is assay undetectable in the central nervous system of older patients with overactive bladder, Int J Clin Pract 64(9):12941300, 2010. Striano P, Striano S: Gabapentin: a Ca2+ channel alpha 2-delta ligand far beyond epilepsy therapy, Drugs Today (Barc) 44(5):353, 2008. Stöhrer M, Mürtz G, Kramer G, et al: Propiverine compared to oxybutynin in neurogenic detrusor overactivity-results of a randomized, double-blind, multicenter clinical study, Eur Urol 51(1):235, 2007. Sugiyama Y, Yoshida M, Masunaga K, et al: Pharmacological effects of propiverine and its active metabolite, M-1, on isolated human urinary bladder smooth muscle, and on bladder contraction in rats, Int J Urol 15(1):76, 2008. Sundin T, Dahlström A, Norlén L, et al: the sympathetic innervation and adrenoreceptor function of the human lower urinary tract in the normal state and after parasympathetic denervation, Invest Urol 14(4):322328, 1977. Sweeney P, Mutambirwa S, Van An N, et al: Flavoxate in the symptomatic treatment of overactive bladder: a meta-analysis, Eur Rev Med Pharmacol Sci 20(17):37033712, 2016. Takao T, Tsujimura A, Yamamoto K, et al: Solifenacin may improve sleep quality in patients with overactive bladder and sleep disturbance, Urology 78(3):648652, 2011. Take H, Shibata K, Awaji T, et al: Vascular alpha1-adrenoceptor subtype selectivity and alpha1-blocker-induced orthostatic hypotension, Jpn J Pharmacol 77(1):6170, 1998. Takeda M, Obara K, Mizusawa T, et al: Evidence for beta3-adrenoceptor subtypes in relaxation of the human urinary bladder detrusor: analysis by molecular biological and pharmacological methods, J Pharmacol Exp Ther 288(3):1367, 1999. Takeda H, Yamazaki Y, Igawa Y, et al: Effects of beta(3)-adrenoceptor stimulation on prostaglandin E(2)-induced bladder hyperactivity and on the cardiovascular system in conscious rats, Neurourol Urodyn 21(6):558, 2002. Takusagawa S, Miyashita A, Iwatsubo T, et al: In vitro inhibition and induction of human cytochrome P450 enzymes by mirabegron, a potent and selective beta3-adrenoceptor agonist, Xenobiotica 42(12):11871196, 2012a. Takusagawa S, Yajima K, Miyashita A, et al: Identification of human cytochrome P450 isoforms and esterases involved in the metabolism ofmirabegron, a potent and selective beta3-adrenoceptor agonist, Xenobiotica 42(10):957 967, 2012c. Tammela T, Kontturi M, Kaar K, et al: Intravesical prostaglandin F2 for promoting bladder emptying after surgery for female stress incontinence, Br J Urol 60:4349, 1987. Tuncel A, Nalcacioglu V, Ener K, et al: Sildenafil citrate and tamsulosin combination is not superior to monotherapy in treating lower urinary tract symptoms and erectile dysfunction, World J Urol 28:1722, 2010. Van de Walle J, Van Herzeele C, Raes A: Is there still a role for desmopressin in children with primary monosymptomatic nocturnal enuresis Van Kerrebroeck P, Kreder K, Jonas U, et al: Tolterodine once-daily: superior efficacy and tolerability in the treatment of the overactive bladder, Urology 57(3):414, 2001. Vande Walle J, Stockner M, Raes A, et al: Desmopressin 30 years in clinical use: a safety review, Curr Drug Saf 2(3):232238, 2007. Vella M, Duckett J, Basu M: Duloxetine 1 year on: the long term outcome of a cohort of women prescribed duloxetine, Int Urogynecol J Pelvic Floor Dysfunct 19(7):961964, 2008. Versi E, Appell R, Mobley D, et al: Dry mouth with conventional and controlledrelease oxybutynin in urinary incontinence. Tanaka Y, Masumori N, Tsukamoto T: Urodynamic effects of solifenacin in untreated female patients with symptomatic overactive bladder, Int J Urol 17(9):796800, 2010. Tatemichi S, Akiyama K, Kobayashi M, et al: A selective alpha1A-adrenoceptor antagonist inhibits detrusor overactivity in a rat model of benign prostatic hyperplasia, J Urol 176(3):12361241, 2006a. Thiagamoorthy G, Giarenis I, Cardozo L: Early investigational 3 adrenoreceptor agonists for the management of the overactive bladder syndrome, Expert Opin Investig Drugs 24(10):12991306, 2015. Thind P, Lose G, Colstrup H, et al: the effect of alpha adrenoceptor stimulation and blockade on the static urethral sphincter function in healthy females, Scand J Urol Nephrol 26:219224, 1992. Thor K, Kirby M, Viktrup L: Serotonin and noradrenaline involvement in urinary incontinence, depression and pain: scientific basis for overlapping clinical efficacy from a single drug, Int J Clin Pract 61(8):13491355, 2007. Tobin G, Sjögren C: In vivo and in vitro effects of muscarinic receptor antagonists on contractions and release of [3H]acetylcholine in the rabbit urinary bladder, Eur J Pharmacol 281:18, 1995. Todorova A, Vonderheid-Guth B, Dimpfel W: Effects of tolterodine, trospium chloride, and oxybutynin on the central nervous system, J Clin Pharmacol 41(6):636, 2001. Wada N, Matsumoto S, Kita M, et al: Improvement of overactive bladder symptoms and bladder ischemia with dutasteride in patients with benign prostatic enlargement, Low Urin Tract Symptoms 7(1):3741, 2015. Wada N, Watanabe M, Kita M, et al: Effect of imidafenacin on nocturia and sleep disorder in patients with overactive bladder, Urol Int 89(2):215221, 2012. Wada N, Watanabe M, Kita M, et al: Efficacy and safety of propiverine and solifenacin for the treatment of female patients with overactive bladder: a crossover study, Low Urin Tract Symptoms 3:3642, 2011. Wagg A, Verdejo C, Molander U: Review of cognitive impairment with antimuscarinic agents in elderly patients with overactive bladder, Int J Clin Pract 64:12791286, 2010. Wagner G, Husstein P, Enzelsberger H: Is prostaglandin E2 really of therapeutic value for postoperative urinary retention Results of a prospectively randomized double blind study, Am J Obstet Gynecol 151:375381, 1985. Walter R, Ullmann C, Thummler D, et al: Influence of propiverine on hepatic microsomal cytochrome p450 enzymes in male rats, Drug Metab Dispos 31(6):714, 2003. Weatherall M: the risk of hyponatremia in older adults using desmopressin for nocturia: a systematic review and meta-analysis, Neurourol Urodyn 23(4):302, 2004. Wehnert J, Sage S: Comparative investigations to the action of Mictonorm (propiverin hydrochloride) and Spasuret (flavoxat hydrochloride) on detrusor vesicae, Z Urol Nephrol 82:259, 1989. Wehnert J, Sage S: Therapie der Blaseninstabilität und Urge-Inkontinenz mit Propiverin hydrochlorid (Mictonorm) und Oxybutynin chlorid (Dridase)- eine randomisierte Crossover- Vergleichsstudie, Actuel Urol 23:7, 1992. Wein A, Malloy T, Shofer F, et al: the effects of bethanechol chloride on urodynamic parameters in normal women and in women with significant residual urine volumes, J Urol 124:397405, 1980a.
Lesions in this location are frequently associated with disturbances of consciousness and respiration blood pressure medication kidney pain 5 mg bystolic with visa, and bladder symptoms may therefore be overlooked. Other regions relevant to bladder control and revealed only by functional imaging include parts of parietal and frontoparietal cortices, posterior cortex (precuneus, posterior cingulate cortex), parts of the limbic system (hippocampal complex, amygdala), and the cerebellum. Functional imaging has occasionally shown activity in the basal ganglia, particularly the striatum and putamen (Griffiths et al. The brain regions involved in bladder control are believed to be organized in neural circuits that perform different tasks related to homeostasis, answering questions regarding the adequacy of bladder filling, and the safety and social appropriateness of voiding, as well as the reflex or mechanical aspects dealt with by the brainstem switch. We should therefore expect forebrain control of the switch to involve limbic circuits (concerned with basic emotion and safety) and cortical circuits (concerned with social propriety [Amodio and Frith, 2006] and conscious decision making). During urine storage, as the bladder fills, it generates afferent signals that are transmitted to the brainstem switch but do not trigger it. Propagation of this insular activity to the lateral and medial prefrontal cortex enables a conscious decision about voiding and an assessment of social propriety and possible embarrassment. If no voiding is planned, a return pathway from the medial frontal cortex to the brainstem tonically suppresses the voiding reflex. The pathway may run directly or via the thalamus in the anterior thalamic radiation. When there is a normal sensation of bladder filling, it exerts negative feedback on the brainstem switch, preventing Physiology and Pharmacology of the Bladder and Urethra 2497 incontinence. During normal daily life, however, there is usually no conscious awareness of the bladder at all. There are at least five receptor subtypes based on molecular cloning and four different receptor subtypes based on pharmacology (M1 to M5) (Eglen et al. Pharmacologically, M1, M2, and M3 receptor subtypes have been found in the human bladder by receptor binding assays (Kondo et al. Although ligand receptor binding studies revealed that M2 receptors predominate, M3 receptors mediate cholinergic contractions (Eglen et al. Working model of forebrain control of micturition showing the brainstem switch and neural circuits that mediate two possible continence mechanisms. The normal mechanism (red) operates when there is a normal sensation of bladder filling. It may operate via brainstem nuclei such as an L-region (pontine storage center) or by modulating the sympathetic input to bladder and urethra. The dashed blue arrows show a possible circuit concerned with monitoring safety and/or maintaining continence without conscious sensation. Studies using constructed mutant mice lacking the M3 receptor or the M2 and M3 receptors have demonstrated that this subtype plays key roles in salivary secretion, pupillary constriction, and detrusor contractions (Igawa et al. In addition, it has also been found that male M3 knockout mice had a distended bladder and larger bladder capacity compared with females, indicating a considerable sex difference in the micturition mechanism (Igawa et al. Oxybutynin is a nonspecific muscarinic antagonist with additional smooth muscle relaxant properties. The smooth muscle relaxation properties of oxybutynin may be clinically relevant only with intravesical instillation of the drug. We will briefly present two additional issues regarding the effect of antimuscarinic drugs on the bladder and salivary glands that have clinical relevancy. First, antimuscarinic drugs are metabolized, and their metabolites have pharmacologic effects. It has been shown that oxybutynin has less of a dry mouth effect than does its metabolite desethyloxybutynin (Gupta and Sathyan, 1999). Smooth muscle relaxants Direct smooth muscle relaxation reduces intravesical pressure during filling and reduces severity and presence of unstable bladder contractions; most of these agents have some degree of anticholinergic action. Act to increase the membrane potential and thus reduce the myogenic initiation of unstable bladder contractions. Prostaglandins have been implicated in increased smooth muscle tone and in the induction of spontaneous activity. Inhibition of prostaglandin synthesis could promote relaxation of the bladder during filling and decrease spontaneous activity of the bladder. Stimulation of -receptors induces relaxation of the bladder body, resulting in a decrease in intravesical pressure during filling. Increase urethral tone and closure pressure by direct stimulation of -adrenergic receptors. Other actions may include increasing adrenergic effects on the urethra and increasing blood flow. Tolterodine and solifenacin have been shown in cats and rats, respectively, to have less activity on the salivary gland muscarinic receptors than on the bladder muscarinic receptors (Nilvebrant et al. Second, the site and speed of antimuscarinic metabolism appear to have profound effects in terms of clinical efficacy and side effects. Muscarinic Selectivity Pharmacologically defined subtype-selective drugs have been developed. Darifenacin and vamicamide have been demonstrated to be relatively selective for the M3 subtype (Andersson, 1997; Steers, 2006; Yamamoto et al. However, they are not necessarily tissue selective, because salivary glands and other tissues also contain M3 muscarinic receptors. Tolterodine appears to be a muscarinic antagonist that has selectivity for the bladder compared with the salivary gland, even though it may not be an M3 subtypeselective antagonist (Andersson, 1998; Nilvebrant et al. Solifenacin has also shown selectivity to the bladder over the salivary gland; the receptor selectivity of solifenacin to M3 receptors over M2 receptors (10-fold) is similar to that of oxybutynin (Ikeda et al. Thus, therapeutically, it is more important to be tissue selective than subtype selective (Andersson, 1998; Nilvebrant et al. Cognitive Impairment With Antimuscarinic Agents It is well established that the efficacy of antimuscarinics and safety profiles depend upon interaction with a variety of muscarinic subtype receptors, which are expressed throughout the body. Studies have revealed that anticholinergic withdrawal is likely to improve central side effects even after only a few weeks.
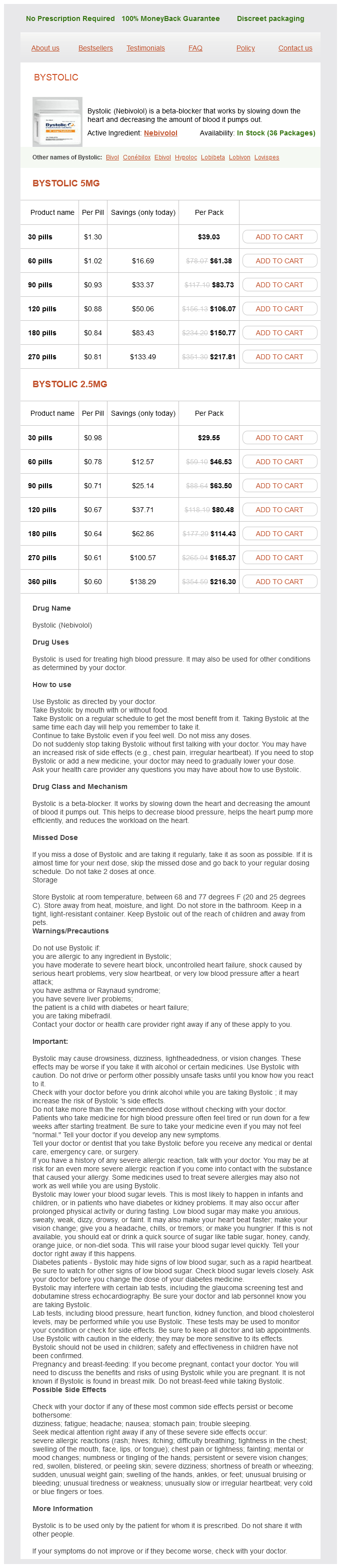
Bystolic Dosage and Price
Bystolic 5mg
- 30 pills - $39.03
- 60 pills - $61.38
- 90 pills - $83.73
- 120 pills - $106.07
- 180 pills - $150.77
- 270 pills - $217.81
Bystolic 2.5mg
- 30 pills - $29.55
- 60 pills - $46.53
- 90 pills - $63.50
- 120 pills - $80.48
- 180 pills - $114.43
- 270 pills - $165.37
- 360 pills - $216.30
However hypertension kidney pathology order discount bystolic online, the published investigations are scarce and the studies are not performed in many patients, so the results should be scrutinized carefully. Most treatment schedules consist of 12 outpatient consecutive treatment sessions lasting 30 minutes each, given 1 to 3 times per week. This schedule implies considerable effort for patients and clinic given 12 weekly outpatient clinic visits. It can be self-administered by the person at home, thus supporting self-management. Moreover it is convenient because the scheme of stimulation is decided entirely by the patient and can therefore reflect personal choices and lifestyle. However, there is a drawback: percutaneous stimulation is more effective than transcutaneous stimulation (George et al. Transcutaneous electrical currents require a higher amplitude because the skin acts as a capacitor, which is often painful. As a consequence the lower amplitude stimulation is used, which results in suboptimal stimulation parameters and effects. The pros and cons of transcutaneous stimulation have been assessed in the systematic review by Booth et al. The studies were very heterogeneous in various ways, had not many participants, and often were underpowered. The stimulation intervention was not standardized across the studies, and a range of dosages were delivered. The duration of treatment program ranged from 4 to 12 weeks, and the total number of included sessions from 5 to 90 (mean 21. The number of weekly sessions varied from daily stimulation to twice weekly and once weekly. Meta-analysis of data from two included studies found a clinically and statistically significant reduction of 3. The best known and best documented Chapter 122 Electrical Stimulation and Neuromodulation in Storage and Emptying Failure 2749 T12 Subcostal Iliohypogastric Ilioinguinal Lat. Structure of the lower lumbar, sacral, and coccygeal nerve plexus, the merger of the various roots and the most important nerves that branches from the merged nerve plexus. L5 S1 S2 S3 S4 S5 Coccygeal Co1 plexus L1 L2 L3 L4 Lumbar plexus Sacral plexus Finazzi-Agro et al. Long-term potentiation or long-term depression of excitatory synaptic transmission can contribute to experience-dependent modifications of brain function, including learning and memory. This suggests that the chronic mechanism of neuromodulation may be due to reorganization of the cortical network. History of Percutaneous Tibial Nerve Stimulation Peripheral neurostimulation is derived from techniques used in traditional Chinese medicine, better known as acupuncture. By puncturing specific points the Chinese attempt to restore "the energetic harmony" of the body. In 1683 a Dutch physician Wilhelmus Ten Rhyne discovered and described this Eastern traditional way of medicine in a book, Dissertatio de Arthritide: Mantissa Schematica: De Acupunctura. In his book he described the technique of "acupunctura" in which needles were used to treat diseases. It is located on the medial side of the lower leg, about 6 to 8 cm cephalad to the prominence of the medial malleolus. When electrical current is applied to the acupuncture needle, the technique is called electrical acupuncture. A network of afferent and efferent fibers is formed after exiting the spinal cord. The sciatic nerve is composed of fibers from L4 to S3 and descends toward the lower extremities (De Groat and Yoshimura, 2015). Neuromodulation is postulated to be the effect of crosssignaling between sympathetic and parasympathetic postganglionic nerve terminals and synapses, causing alteration of efferent nerve signals from the spinal cord to the bladder. Stimulation of peripheral nerves and subsequent "cross-talk" at the level of the postganglionic neuroeffector junctions can modulate efficiency of transmission. The pudendal nerve, the dorsal genital nerve, and the posterior tibial nerve are examples of such peripheral nerves. This implies that stimulating one area of the innervations system may influence nerve behavior of other systems, which, for example, may change bladder behavior. A 34-gauge stainless steel needle is inserted approximately 3 to 4 cm, or 3 fingerbreadths, cephalad to the medial malleolus, between the posterior margin of the tibia and soleus muscle with an angulation of 60 degrees to 90 degrees. The tip of the needle has to be juxtaposed with the tibial nerve without actually touching it. The needle and grounding pad are connected to a low-voltage (9 volts) stimulator with an adjustable pulse intensity of 0 to 10 mA, a fixed pulse width of 200 microseconds, and a frequency of 20 Hz. Once optimal position is ensured, stimulation is applied at an tolerable intensity level. Based on studies most treatment schedules consist of 12 outpatient consecutive treatment sessions lasting 30 minutes given once to three times per week (Peters et al. These patients were prescribed a fixed-schedule 14-week tapering protocol followed by a personal treatment. Of this group 29 patients completed the 36-month protocol receiving a median of 1. In 71% of patients, symptoms improved and low scores on the visual analog scale for pain were noted, which even decreased further during the treatment period (De Gennaro et al. Technique of percutaneous tibial nerve stimulation with needle at the tibial nerve, the ground pad electrode, and the stimulator. Overall subjective success, defined as improved QoL or willingness to continue treatment, was found in 56% to 64%. This was the first study including a validated sham arm to provide more information on the placebo effect.
© 2025 Adrive Pharma, All Rights Reserved..