General Information about Butenafine
One of the major advantages of Butenafine is its low likelihood of inflicting unwanted aspect effects. This is as a result of of its targeted motion on the fungal cells, making it safe for use even on delicate pores and skin. Some of the widespread unwanted effects that may happen embody gentle burning or stinging sensation on the utility web site, itching, and dryness. However, these unwanted effects are usually delicate and subside within a number of days of use. In uncommon cases, allergic reactions could occur, however they're unusual.
One of essentially the most commonly treated fungal infections with Butenafine is athlete's foot, also referred to as tinea pedis. This infection is brought on by a fungus referred to as Trichophyton, which thrives in heat and moist environments similar to swimming swimming pools, locker rooms, and public showers. Athlete's foot could cause itching, burning, and redness on the affected skin, especially between the toes. It can even unfold to different areas, such as the toenails and palms. Butenafine is highly efficient in treating athlete's foot and may present relief from signs inside a number of days of use.
Butenafine is on the market as a topical cream and must be applied to the affected space once a day. The length of remedy can range depending on the kind and severity of the fungal an infection. It is essential to observe the directions offered by the physician or as mentioned on the product label. It can also be advisable to continue utilizing the cream for the prescribed period, even when the signs improve, to stop the infection from coming again.
In conclusion, Butenafine, also called Mentax, is a extremely efficient and protected treatment for treating fungal infections of the pores and skin. Its dual-mode of action makes it more potent than different antifungal medicine, and it is well-tolerated by most individuals. However, like all treatment, it's essential to make use of Butenafine as directed and to consult a physician if any unwanted effects happen. So, if you're suffering from a fungal infection, it's best to consult a healthcare professional and consider using Butenafine for fast and efficient reduction.
Butenafine is an artificial antifungal treatment that belongs to the category of medicine known as allylamines. It works by stopping the growth of fungi on the skin, thus eliminating the an infection. Unlike different antifungal medications, Butenafine has a dual-mode of action, making it more effective in treating a broad range of fungal infections. It not only stops the expansion of the fungi but in addition prevents them from multiplying. This helps in decreasing the possibilities of reinfection and hastens the therapeutic process.
Fungal infections are a common downside that can have an effect on anybody regardless of age, gender, or race. They can vary from delicate skin rashes to more serious infections that require medical treatment. One such medication that is extensively used for treating fungal infections of the pores and skin is Butenafine, also identified by its model name Mentax. This topical cream is very efficient in treating a selection of fungal infections and has gained popularity amongst each patients and healthcare professionals.
Butenafine is also used to deal with different fungal infections, such as jock itch (tinea cruris) and ringworm (tinea corporis). These infections are caused by fungi that could be spread through direct contact with an infected person or animal or by touching contaminated surfaces. They are characterized by an itchy, purple, and scaly rash on the affected area. Butenafine can effectively remove these infections and prevent them from recurring.
Individuals who may respond less well to operative therapy include those with atypical symptoms and those who have esophageal body motor disturbances antifungal nasal spray prescription buy generic butenafine line. Dysphagia, gasbloat syndrome, and gastroparesis may be long-term complications of these procedures. Some patients with functional heartburn and functional dyspepsia refractory to standard therapies may respond to low-dose antidepressants in tricyclic and other classes. Their mechanism of action is unknown but may involve blunting of visceral pain processing in the brain. Gas and bloating are among the most troubling symptoms in some patients with indigestion and can be difficult to treat. Dietary exclusion of gas-producing foods such as legumes and use of simethicone or activated charcoal provide benefits in some cases. Therapies that modify gut flora, including antibiotics and probiotic preparations containing active bacterial cultures, are useful for cases of bacterial overgrowth and functional lower gastrointestinal disorders, but their utility in functional dyspepsia is unproven. Psychological treatments may be offered for refractory functional dyspepsia, but no convincing data suggest their efficacy. The utility of eradication therapy in functional dyspepsia is less well established, but <15% of cases relate to this infection. Several studies have evaluated the effectiveness of motor-stimulating drugs in functional dyspepsia; however, convincing evidence of their benefits has not been found. Some clinicians suggest that patients with symptoms resembling postprandial distress may respond preferentially to prokinetic drugs. Murray Diarrhea and constipation are exceedingly common and, together, exact an enormous toll in terms of mortality, morbidity, social inconvenience, loss of work productivity, and consumption of medical resources. Worldwide, >1 billion individuals suffer one or more episodes of acute diarrhea each year. Acute infectious diarrhea remains one of the most common causes of mortality in developing countries, particularly among children, accounting for 23 million deaths per year. Constipation, by contrast, is rarely associated with mortality and is exceedingly common in developed countries, leading to frequent self-medication and, in a third of those, to medical consultation. United States population surveys put prevalence rates for chronic diarrhea at 27% and for chronic constipation at 1219%, with women being affected twice as often as men. Diarrhea and constipation are among the most common patient complaints faced by internists and primary care physicians, and they account for nearly 50% of referrals to gastroenterologists. Even mild symptoms may signal a serious underlying gastrointestinal lesion, such as colorectal cancer, or systemic disorder, such as thyroid disease. Given the heterogeneous causes and potential severity of these common complaints, it is imperative for clinicians to appreciate the pathophysiology, etiologic classification, diagnostic strategies, and principles of management of diarrhea and constipation, so that rational and cost-effective care can be delivered. Alterations in fluid and electrolyte handling contribute significantly to diarrhea. The myenteric plexus regulates smooth-muscle function, and the submucosal plexus affects secretion, absorption, and mucosal blood flow. The parasympathetic nerves convey visceral sensory and excitatory pathways to the colon. Parasympathetic fibers via the vagus nerve reach the small intestine and proximal colon along the branches of the superior mesenteric artery. The distal colon is supplied by sacral parasympathetic nerves (S24) via the pelvic plexus; these fibers course through the wall of the colon as ascending intracolonic fibers as far as, and in some instances including, the proximal colon. The sympathetic nerve supply modulates motor functions and reaches the small intestine and colon alongside their arterial vessels. Sympathetic input to the gut is generally excitatory to sphincters and inhibitory to nonsphincteric muscle. Other afferent fibers synapse in the prevertebral ganglia and reflexly modulate intestinal motility. A variety of neural and non-neural mediators regulate colonic fluid and electrolyte balance, including cholinergic, adrenergic, and serotonergic mediators. Angiotensin and aldosterone also influence colonic absorption, reflecting the common embryologic development of the distal colonic epithelium and the renal tubules. This organized, propagated series of contractions last, on average, 4 min, occur every 6090 min, and usually involve the entire small intestine. After food ingestion, the small intestine produces irregular, mixing contractions of relatively low amplitude, except in the distal ileum where more powerful contractions occur intermittently and empty the ileum by bolus transfers. IleocolonIc storage and salvage the distal ileum acts as a reservoir, emptying intermittently by bolus movements. There is increased appreciation of the intimate interaction between the colonic function and the luminal ecology. The resident bacteria in the colon are necessary for the digestion of unabsorbed carbohydrates that reach the colon even in health, thereby providing a vital source of nutrients to the mucosa. In health, the ascending and transverse regions of colon function as reservoirs (average transit, 15 h), and the descending colon acts as a conduit (average transit, 3 h). The colon is efficient at conserving sodium and water, a function that is particularly important in sodium-depleted patients in whom the small intestine alone is unable to maintain sodium balance. Diarrhea or constipation may result from alteration in the reservoir function of the proximal colon or the propulsive function of the left colon. Constipation may also result from disturbances of the rectal or sigmoid reservoir, typically as a result of dysfunction of the pelvic floor, the anal sphincters, or the coordination of defecation. Thus, the colon can partially compensate for excess fluid delivery to the colon because of intestinal absorptive or secretory disorders. The predominant phasic contractions in the colon are irregular and nonpropagated and serve a "mixing" function. As sigmoid and rectal contractions increase the pressure within the rectum, the rectosigmoid angle opens by >15°.
In the United States antifungal resistant ringworm purchase butenafine 15 mg with mastercard, the mortality rate of patients on dialysis is approximately 1820% per year, with a 5-year survival rate of approximately 3035%. Deaths are due mainly to cardiovascular diseases and infections (approximately 50 and 15% of deaths, respectively). Older age, male sex, nonblack race, diabetes mellitus, malnutrition, and underlying heart disease are important predictors of death. In contrast to hemodialysis, peritoneal dialysis is continuous but much less efficient, in terms of solute clearance. While no large-scale clinical trials have been completed comparing outcomes among patients randomized to either hemodialysis or peritoneal dialysis, outcomes associated with both therapies are similar in most reports, and the decision of which modality to select is often based on personal preferences and quality-of-life considerations. In addition to diffusive clearance, movement of waste products from the circulation in to the dialysate may occur as a result of ultrafiltration. The Dialyzer There are three essential components to hemodialysis: the dialyzer, the composition and delivery of the dialysate, and the blood delivery system. The dialyzer is a plastic chamber with the ability to perfuse blood and dialysate compartments simultaneously at very high flow rates. The surface area of modern dialysis membranes in adult patients is usually in the range of 1. These dialyzers are composed of bundles of capillary tubes through which blood circulates while dialysate travels on the outside of the fiber bundle. Recent advances have led to the development of many different types of membrane material. Broadly, there are four categories of dialysis membranes: cellulose, substituted cellulose, cellulosynthetic, and synthetic. Over the past three decades, there has been a gradual switch Acid concentrate Na+ Cl K+ Acetate Ca2+ Mg2+ Hemodialysis Section iii Acute Kidney injury and chronic Renal Failure Hemodialysis relies on the principles of solute diffusion across a semipermeable membrane. The rate of diffusive transport increases in response to several factors, including the magnitude of the concentration gradient, the membrane surface area, and the mass transfer coefficient of the membrane. The latter is a function of the porosity and thickness of the membrane, the size of the solute molecule, and the conditions of flow on the two sides of the membrane. Cellulosic membranes are bioincompatible because of the presence of free hydroxyl groups on the membrane surface. Synthetic membranes, such as polysulfone, polymethylmethacrylate, and polyacrylonitrile membranes, are even more biocompatible because of the absence of these hydroxyl groups. The majority of dialyzers now manufactured in the United States are derived from polysulfone or newer derivatives (polyarylethersulfone). Reprocessing and reuse of hemodialyzers are often employed for patients on maintenance hemodialysis in the United States. However, as the manufacturing costs for disposable dialyzers have declined, more and more outpatient dialysis facilities are no longer reprocessing dialyzers. In most centers employing reuse, only the dialyzer unit is reprocessed and reused, whereas in the developing world blood lines are also frequently reused. It consists of the sequential rinsing of the blood and dialysate compartments with water, a chemical cleansing step with reverse ultrafiltration from the dialysate to the blood compartment, the testing of the patency of the dialyzer, and, finally, disinfection of the dialyzer. Formaldehyde, peracetic acidhydrogen peroxide, glutaraldehyde, and bleach have all been used as reprocessing agents. Higher dialysate sodium concentrations and sodium modeling may predispose patients to positive sodium balance; thus, these strategies to ameliorate intradialytic hypotension may be undesirable in hypertensive patients or in patients with large interdialytic weight gains. Because patients are exposed to approximately 120 L of water during each dialysis treatment, water used for the dialysate is subjected to filtration, softening, deionization, and, ultimately, reverse osmosis. During the reverse osmosis process, water is forced through a semipermeable membrane at very high pressure to remove microbiologic contaminants and >90% of dissolved ions. The blood pump moves blood from the access site, through the dialyzer, and back to the patient. The blood flow rate may range from 250500 mL/min, depending largely on the type and integrity of the vascular access. Negative hydrostatic pressure on the dialysate side can be manipulated to achieve desirable fluid removal or ultrafiltration. The dialysis solution delivery system dilutes the concentrated dialysate with water and monitors the temperature, conductivity, and flow of dialysate. Dialysis in the treatment of Renal Failure DialySaThe the potassium concentration of dialysate may be varied from 0 to 4 mmol/L depending on the predialysis serum potassium concentration. Lower dialysate sodium concentrations are associated with a higher frequency of hypotension, cramping, nausea, vomiting, fatigue, and dizziness in some patients, although may attenuate thirst. In patients who frequently develop hypotension during their dialysis run, "sodium modeling" to counterbalance urea-related osmolar gradients is often employed. In recent years, nephrologists, vascular surgeons, and health care policy makers in the United States have encouraged the creation of arteriovenous fistulas in a larger fraction of patients (the "fistula 144 first" initiative). Grafts and catheters tend to be used among persons with smaller-caliber veins or persons whose veins have been damaged by repeated venipuncture, or after prolonged hospitalization. The most important complication of arteriovenous grafts is thrombosis of the graft and graft failure, due principally to intimal hyperplasia at the anastomosis between the graft and recipient vein. When grafts (or fistulas) fail, catheter-guided angioplasty can be used to dilate stenoses; monitoring of venous pressures on dialysis and of access flow, although not routinely performed, may assist in the early recognition of impending vascular access failure. Intravenous large-bore catheters are often used in patients with acute and chronic kidney disease.
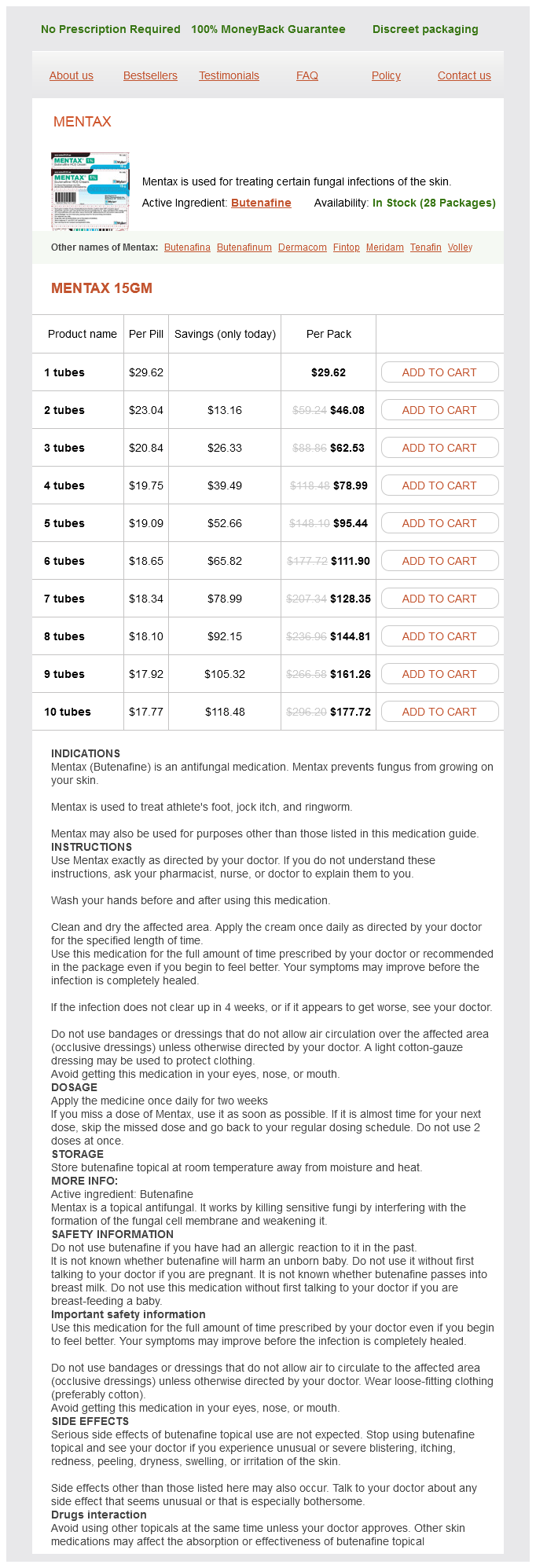
Butenafine Dosage and Price
Mentax 15gm
- 1 tubes - $29.62
- 2 tubes - $46.08
- 3 tubes - $62.53
- 4 tubes - $78.99
- 5 tubes - $95.44
- 6 tubes - $111.90
- 7 tubes - $128.35
- 8 tubes - $144.81
- 9 tubes - $161.26
- 10 tubes - $177.72
Carina: It is a triangular hook shaped process in the last ring of trachea curving downwards and backwards fungus armpit 15 mg butenafine sale. Development Trachea develops from the intermediate part of the laryngotracheal tube. Tracheoesophageal fistula: It is the congenital anomaly where communication occur between the bifurcation of trachea and the esophagus. Carina present in the last ring of trachea which helps in bronchoscopic examination. Foreign body in trachea: Any foreign body through the trachea will enters in to the right 4. Tracheostomy: It is done by a midline vertical incision with isthmus of the thyroid gland retracted inferiorly. Insertion At the central tendon, situated in the middle depressed part of the diaphragm near the sternum. Effects of contraction: During contraction of the diaphragm in inspiration this opening dilates and helps in venous return. Esophageal opening Situation: It is located in the muscular part of the diaphragm. Effects of contraction: During inspiration the opening is constricted, which prevents regurgitation of contents of stomach in to the esophagus. Aortic opening Situation: Vertebral level: Lower border of T12 vertebra, slightly left to the midline. Shape Its thoracic surface is convex on right and left but in the middle it is depressed and concave in its inferior or abdominal surface. Costal: From the inner surface of the lower 6 ribs with respective cartilages, interdigitating with transversus abdominis. Right crus: It is longer and also more muscular comparatively than the left crus Origin: From the front of the bodies and intervertebral disks of L1 to L3 vertebrae. From a pair of medial arcuate ligaments, which is attached to the side of body of L1 or L2 vertebrae and laterally to the tip of the transverse process of L1 vertebra iii. It is attached medially to the tip of the transverse process of the L1 vertebra and laterally to the lower border of 12th ribs near its mid point. Space of Larrey: It is a triangular gap between sternal origin and 7th costal cartilage. Foramen Morgagni: the enlarged opening of the space of Larrey is called foramen Morgagni. Between the digitations of costal origins of the diaphragm and transversus abdominis. Between the origin of 7th and 8th costal cartilages Structures passing through it: Musculophrenic vessels. Sometimes remnant suprahepatic part of vitelline vein (between median and left leaflets). Sometimes foramen Morgagni may be enlarged cause abdominal viscera to herniate in to the thorax. Irritation of diaphragm may cause referred pain to shoulder due to same segmental nerve supply. Acquired hiatus hernia: It is the commonest of all internal hernia, due to the weakness of phrenoesophageal ligament. It helps in expulsive function during the act of vomiting, micturition, defecation and parturition. It may arise from the back of inferior vena cava at or below the renal vein as lumbar azygos vein. It may formed by the union of the right subcostal and right ascending lumbar veins. Right superior intercostal vein formed by second, third and fourth right posterior intercostal veins ends in to arch of azygos vein ii. In the thorax the azygos vein passes upwards, anterior to the lower 8 thoracic vertebrae lying right of the thoracic duct and descending thoracic aorta. Sometimes arch of the vein splits near the apex of right lung and lodges in a fissure. Lower 8 thoracic vertebrae, with intervertebral disks and anterior longitudinal ligament ii. Beginning with level It is formed by the union of right and left brachiocephalic veins behind the lower border of right first costal cartilage close to the manubrium sterni. After its formation, it descends vertically with slight convexity to the right behind the first and second right intercostal spaces ii. In its course, it pierces the fibrous pericardium at the level of right 2nd costal cartilage which causes the superior vena cava divides in to extrapericardial and intrapericardial parts iii. Lastly, it drains in to the posterosuperior part of the right atrium behind right 3rd costal cartilage. The obstruction may occur above the opening of azygos vein or below the opening of azygos vein. If obstruction occur above the opening of azygos vein the venous blood return from upper part of the body through the azygos vein result is superficial veins are dilated on chest wall. If obstruction occurs below the azygos vein venous blood will returned through the inferior vena cava via the femoral veins result is superficial veins of the chest wall and abdomen up to the saphenous opening of the thigh dilated. The signs depend on the obstruction and collateral circulation which are given below: i. Via the azygos vein: It directly connects the superior vena cava with the inferior vena cava. Hyposthenic or asthenic type: Here J is vertical, this type of stomach prone to suffer from gastric ulcer.
© 2025 Adrive Pharma, All Rights Reserved..