General Information about Buspirone
It is important to notice that Buspirone could take a couple of weeks to start working, in contrast to another medicines that may have immediate results. This is as a end result of it works via a gradual buildup of serotonin in the mind, as opposed to concentrating on specific neurotransmitters. Therefore, it is necessary to proceed taking Buspirone as prescribed, even if you do not see quick outcomes. Additionally, abruptly stopping Buspirone can lead to withdrawal signs, so you will need to consult along with your doctor before discontinuing use.
Buspar is primarily prescribed for generalized anxiety dysfunction (GAD), however it can additionally be used to treat other anxiousness issues such as panic disorder and social anxiousness disorder. It is commonly prescribed together with remedy and different behavioral methods to handle nervousness symptoms.
In conclusion, Buspirone is a safe and effective medication for treating nervousness issues. Its distinctive mechanism of action, minimal unwanted aspect effects, and lack of dependence make it a well-liked alternative for these on the lookout for aid from anxiety. However, you will want to remember that medication alone isn't sufficient in managing nervousness and ought to be used in conjunction with therapy and life-style changes for the most effective results. As at all times, it's essential to seek the guidance of with a healthcare skilled before starting any new treatment.
While Buspirone is generally well-tolerated, it isn't suitable for everybody. Pregnant or breastfeeding ladies, as well as these with a history of liver or kidney illness, ought to seek the advice of with their physician earlier than taking this treatment. It could work together with other medicines, so you will need to disclose all current medicines and supplements to your doctor before starting Buspirone.
Buspirone, also identified by its model name Buspar, is a medication generally used to deal with anxiety problems. It belongs to a class of medicine referred to as serotonin receptor agonists, which work by binding to sure receptors within the mind and activating the manufacturing of serotonin, a neurotransmitter responsible for regulating temper. Unlike different antidepressants, Buspirone does not work on the degrees of chemicals like serotonin and dopamine within the brain, but somewhat on the receptors that these chemical substances signal to. This distinctive mechanism of action makes Buspirone a preferred alternative for individuals who haven't found aid from conventional antidepressants.
One of the major benefits of Buspirone is that it usually doesn't trigger as many unwanted effects as other drugs used to treat anxiousness. It doesn't lead to sedation, cognitive impairment, or dependence, making it a safer choice for long-term use. However, like several medicine, Buspirone can cause side effects similar to dizziness, nausea, and headaches, however these are usually delicate and momentary.
Furthermore anxiety symptoms heart rate buy cheap buspirone 10 mg online, larger/irregular-shaped particles (6 m) that can be phagocytosed have showed the greatest lysosomal destabilisation and inflammatory reactivity compared to smaller/spherical (1 m) particles in vitro [79]. However, they have also specified that simply increasing implant size might be insufficient, meaning that spherical shape was also integrated with size [81]. Another major feature that should be primarily introduced to optimise bone biomaterials is creating a pore network and porosity on scaffolds. This process is especially important for prompting in vivo tissue growth or regeneration processes [82,83]. Scaffold porosity allows vascularisation, thus enables the transportation of fundamental nutrients and gases while clearing away metabolic wastes [83,84]. This restricts the transportation of nutrients and oxygen as well as matrix elaboration within the scaffolds [84,86,87]. Oxygen deficiency gives rise to a hypoxic environment at the injury site, which in turn may enhance inflammation. Several studies have reported that small pore sizes (75100 m) induces chondrogenesis due to the low oxygen tension, while large pore sizes (>300 m) induce osteogenesis as a result of enhanced vascularisation, which result in the transportation of nutrients and a high degree of oxygen [86,89,90]. As a result, the subsequent events such as cell proliferation and differentiation will be hampered [86,87]. Moreover, the combination of higher porosity (around 80%) and macro-porosity is also believed to enhance osteogenesis due to successful nutrient delivery, vascularisation and tissue regeneration. They observed that scaffolds were biocompatible and none of them showed any foreign body reactions [92]. Many researchers have focused on porous scaffolds made of ceramics, composites, polymers and metals. Studies on pore size and porosity show that immune system may give different responses to distinctive materials with varied pore sizes and porosity. Surface topography and micro-/nanoscale architecture modulate cell adhesion, proliferation and spreading while directing immune cell interaction. For improving tissue remodelling rather than only supporting the injury site, the chosen scaffold should mimic the natural bone surface roughness. Similarly, immune response also depends on the topographic structure of the surface even more than its chemical properties. Macrophage spreading enhanced with increasing surface roughness and the highest spreading observed on grit-blasted surfaces. Moreover, they concluded that surface roughness modulated the expression of cytokines [95]. They concluded that there was a decrease in monocyte, macrophage and neutrophil functionality on titania nanotube arrays as compared to biomedical-grade titanium, which was evidence that nanoarchitecture has high potential for biomedical applications [96]. Surface energy and wettability are also considerable properties that influence the adsorption kinetics and conformation characteristics of the proteins, eventually affecting inflammatory responses. Hydrophilic surfaces thermodynamically tend to adsorb lower amounts of protein in comparison to hydrophobic surfaces. Hence, the reduction in cell responses to hydrophilic surfaces evokes less immune reaction in the body. In this regard, they concluded that bone resorption with hydrophilic surfaces might evoke inflammatory responses [97]. On the other part, hydrophobic surfaces cause an increase of fibrinogen, IgG and non-specific antibodies adsorption on the material surface, as well as an increase in coagulation factors [99]. In this scenario, the change in the conformation of fibrinogen initiates platelet adhesion, as well as the recruitment of macrophages and their fusion into foreign body giant cells by exposing their hidden domains (D domain) as a ligand for inflammatory cell receptors [100102]. Surface charge and chemistry have considerable influences on protein adsorption, denaturation and subsequent cellular responses. Surface functionality with hydrophilic or neutral groups is more favourable than hydrophobic functionality. In the case of charge properties, it has been proven that fibrinogen prefers hydrophobic and positively charged surfaces instead of hydrophilic and negatively charged surfaces [99,101]. Brodbeck also reported that hydrophilic and anionic surfaces showed an anti-inflammatory type of response by dictating selective cytokine production by adherent monocytes and macrophages [106]. In the same manner, these elements and molecules can be manipulated to modulate immune responses. Some inorganic ions, such as Ca, Co, Cu, Mg, P, Si, Sr and Zn, are common elements that are involved in bone metabolism. These elements are also incorporated into biomaterials as ionic dissolution products to affect the behaviour of cells, in addition to increase bioactivity. Thus, the solution of these materials in the physiological environment and the participation of dissolved ions to different pathways may stimulate new bone formation upon the activation of osteoblast cells and suppression of the immune system. Moreover, well-ordered mesopore channel structures of the scaffold have succeeded at controllable antibiotic release. Although it also has a role on collagen synthesis and matrix mineralisation, the biological reaction of Si is not yet fully understood [111]. Zinc is another essential trace element that plays an important role in the metabolic pathways of bone and the immune system [112]. Day and Boccaccini have put an emphasis on the ionic dissolution of silicate- and zinc phosphate-based bioactive glasses and, as associated with this, cytokine release from human macrophages and monocytes. The degradation of scaffolds accompanying ion dissolution changes the surrounding environment and may elicit or reduce immune response. Therefore, optimisation and refined fabrication of scaffolds that are combined with ions in appropriate concentration is of great importance. Most recent biomaterial studies have been focused on introducing growth factors to biomaterials to realise these molecular and cellular activities, along with the modulation of inflammatory reactions. This protein plays an important role in the formation of blood vessels and endothelial cell activity.
The requirement is for one nurse to every four babies Provide high-dependency care and some short-term intensive care as agreed within the network anxiety symptoms for no reason generic 5 mg buspirone visa. This requires one trained nurse to two babies Provide the whole range of medical neonatal care but not necessarily all specialist services such as neonatal surgery. The mature infant nursery provides basic life supports and receives back transfer from level 2 hospitals Level 2 (4002000 deliveries per annum). These provide services for low-, medium- and hospitals high-risk obstetrics, have a maternal fetal medicine unit and a full range of ventilation options. The staff include neonatal nurses, neonatal registrars and a consultant, and there is access to a full range of paediatric subspecialties. There is a nurse:patient ratio of 1:2, or 1:1 for unstable infants Level 4 this is a term that is sometimes used to describe services provided to neonates requiring paediatric hospitals subspecialty care. Special care is provided for all other babies who could not reasonably be expected to be looked after at home by their mother. Normal care is care given in a postnatal ward, usually by the mother under the supervision of a midwife or doctor, but requiring minimal medical or nursing advice. Any baby receiving respiratory support via a tracheal tube and in the first 24 hours after withdrawal of such support. Presence of a replogle tube, epidural catheter, extraventricular drain, silo for gastroschisis. Babies requiring major emergency surgery, for the preoperative period and postoperatively for 24 hours. Babies requiring complex clinical procedures: full exchange transfusion, peritoneal dialysis. Baby requires infusion of an inotrope, insulin, pulmonary vasodilator or prostaglandin. Any other very unstable baby considered by the nurse in charge as needing one-to-one nursing. Babies over 1000 g current weight and not fulfilling any of the criteria for intensive care. Babies requiring specified procedures that do not fulfil any criteria for intensive care: care of an intra-arterial catheter or chest drain; partial exchange transfusion; tracheostomy care until supervised by a parent. A district general hospital with a consultant obstetric unit should provide special care facilities, and approximately 6% of infants will require this type of care. Neonatal services should be developed to oversee a continuum of care between the different levels, hospitals and community-based primary health facilities. It is essential that effective communication occurs as babies and their families transition between services. Neonatal networks Collaboration with a regional, national or international neonatal network audits outcomes, provides benchmarking standards, develops clinical indicators, provides standardized guidelines and policies, allows consultation with the referring and receiving units, and facilitates research through critical mass. Therefore, if possible, the birth of a high-risk infant should occur in a hospital capable of providing the necessary care. If birth occurs in a place without the required facilities, the infant should be stabilized and transferred to an appropriate higher-level centre within the service network. Transport in utero the ideal time to transfer a potentially sick infant is in utero, if the problem can be anticipated. High-risk pregnancies should be transferred before delivery, and a high-risk fetus should be transferred in utero to a unit with perinatal intensive care facilities. In all cases there must be consultation with the receiving hospital before transfer. Unfortunately, not all neonatal problems can be recognized from an at-risk pregnancy, and some women are unwilling to be transported before delivery. The incidence of intraventricular haemorrhage in infants born in a referring hospital after in-utero transfer is significantly lower than in a similar group of outborn babies. The decision to transfer a sick neonate will depend on the expertise of the intensive care nursery, the safety of travel, and the facilities available at the hospital where the baby was born. Discussion with a neonatal paediatrician may obviate the need for transport or provide advice on the best methods of transfer. Personnel from the neonatal emergency transport service can assist with the decision on whether transfer is necessary. Consideration should be given to the transfer of any infant if the facilities do not exist in the admitting hospital. Oxygen requirement >50% or associated apnoea, meconium aspiration or suspected pneumonia. It is also influenced by the distance to be travelled, the duration of the journey, and the mode of transport. Staff must be aware of the difficulties of detecting and correcting problems in transit, and must ensure appropriate stabilization before transport. The infant should be resuscitated and his/her condition stabilized prior to transport. While awaiting transfer the referring hospital should provide the following care: the infant is kept warm (ideally servocontrolled to a skin temperature of 37 °C). The infant is given sufficient oxygen to maintain oxygen saturation in the range of 9195% for preterm infants and 94% for term infants (target may be lower in certain conditions). Adequate respiration is ensured (some babies will require additional respiratory support. The baby is not fed during transport and the stomach is aspirated before leaving the referring hospital. Frequent observations of temperature, heart rate, respiratory rate, blood pressure and blood sugar by reagent stick. Other specific conditions will require additional treatments on advice from the retrieving centre.
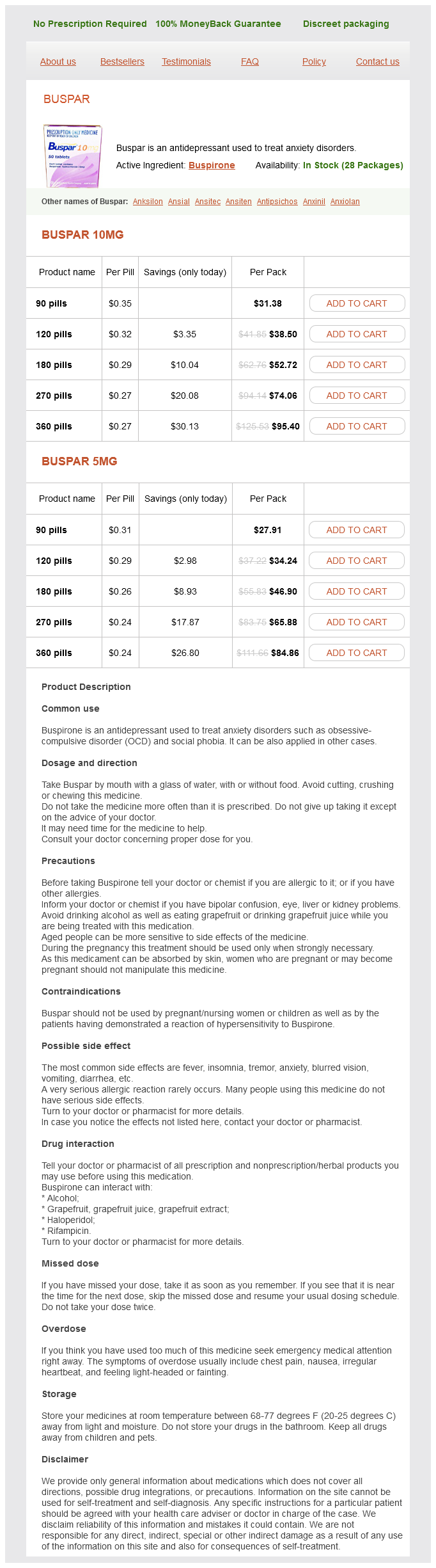
Buspirone Dosage and Price
Buspar 10mg
- 90 pills - $31.38
- 120 pills - $38.50
- 180 pills - $52.72
- 270 pills - $74.06
- 360 pills - $95.40
Buspar 5mg
- 90 pills - $27.91
- 120 pills - $34.24
- 180 pills - $46.90
- 270 pills - $65.88
- 360 pills - $84.86
A fetotoxin is an agent causing damage of any kind to the fetus anxiety dreams generic buspirone 5 mg buy online, and a mutagen is an agent that causes a permanent transmissible change in the genetic material. The commonest potential teratogens are medications, and so in general drugs should be avoided during pregnancy and, if essential, their safety profile must be checked before prescribing. Unfortunately, with some newer agents human safety data is lacking and animal data must be used to make a careful riskbenefit assessment. This is why congenital anomaly registers are important, to identify unexpected clusters of congenital anomalies. The critical periods in embryogenic development have been extrapolated from the effects of rubella exposure, and are expressed in days from time of conception (not last menstrual period) in Table 4. Organ Risk period (days after conception) Brain Eye Heart Limbs Ear 1525 2540 2040 2436 4060 During the first 2 weeks of development from conception to the first missed period the embryo is resistant to any teratogenic effects of medicines. The critical period begins when organ development starts at 17 days after conception, and extends until this is complete at 6070 days. In general, exposure to medicines beyond 70 days after conception is not associated with major birth defects. However, drugs can interfere with functional development of organ systems in the second and third trimesters. Pharmaceutical agents Drugs may act by interfering with embryogenesis or by exerting their pharmacological actions on developing fetal organs. The timing and dose of agent, the efficiency with which the mother metabolizes the agent, placental transfer and the individual susceptibility of the fetus are important. Hormones Progestogens, diethyl stilboestrol, male sex hormones Antipsychotics, hypnotics, anticonvulsants Lithium, haloperidol, thalidomide Anticonvulsants Antimicrobials Antineoplastics Anticoagulants Antithyroids Antivirals Hypoglycaemics Vitamin A analogues Others Hydantoins, sodium valproate, carbamazepine, primidone, phenobarbitone Tetracycline, chloramphenicol, streptomycin, flucytosine, amphotericin B Alkylating agents, folic acid antagonists Warfarin Iodine, carbimazole, propylthiouracil Ribavirin Biguanides, sulphonylureas Isotretinoin, etretinate Toluene, alcohol, marijuana, narcotics Irradiation Exposure to radiation in pregnancy is now rare, but previous experience with X-rays, atomic bomb irradiation and nuclear accidents confirmed major teratogenic effects, including microcephaly. Chemicals Pesticides and waste products have not been subjected to rigorous teratogenic studies in humans. However, experience with the dioxin contaminant in the insecticide 2,4,5-T and its possible association with spina bifida and Potter,s syndrome suggest that rigorous surveillance of chemicals is necessary. Long-term prenatal exposure to organic mercury causes disturbed brain development. Methyl isocyanate gas released in the Bhopal disaster led to an increase in congenital anomalies in the offspring of those exposed (mutagenic effect). Congenital malformation secondary to maternal infections Prenatal infections cause inflammation which interferes with cell division. Sauna baths and faulty electric blankets producing very high body temperatures at a critical period of embryogenesis may be teratogenic. Consequences of maternal substance misuse All drug ingestion during pregnancy carries risk to the developing fetus, and maternal substance misuse can cause fetal malformation and sometimes neonatal withdrawal. Cigarettes, alcohol, opiates, amphetamines and cocaine are all known to cause harm. Excessive alcohol intake during fetal organogenesis can result in a specific syndrome of facial abnormalities, growth failure, microcephaly and skeletal and visceral abnormalities. Major abnormalities include cleft lip and palate, and limb, ocular, cardiac and renal malformations. Approximately one-third of infants born to chronic alcoholic women develop the fetal alcohol syndrome, whereas others may be growth-restricted or demonstrate only minor features. However, current recommendation is to avoid all alcohol consumption during pregnancy. Diagnosis relies on a pattern of abnormalities that makes up the disorder, along with a history of alcohol misuse during pregnancy. Various scoring systems are in use, such as the four-digit diagnostic code (see Box 4. Extreme tremulousness and seizures may occur and can be controlled with phenobarbitone. Smoking in pregnancy Although there is overwhelming evidence of harm to the fetus and mother from smoking, up to 15% of pregnant women still smoke. Smoking has a dose-dependent effect on growth due to impaired uterine perfusion, with placental changes, increased carboxyhaemoglobin levels and increased fetal erythropoiesis. Complications in smokers include subfertility, spontaneous abortion, impaired fetal growth, placenta praevia, placental abruption, amniotic fluid infection and premature rupture of the membranes. Infants of substance-misusing mothers Neonatal withdrawal symptoms have been reported with alcohol, amphetamines, barbiturates, codeine, ethchlorvynol, heroin, pethidine, methadone, morphine and pentazocine. Opiate use in pregnancy Heroin and methadone are the narcotic drugs most frequently abused during pregnancy. The fetal brain becomes acclimatized to the chronic stimulation of opiate receptors in the brainstem. Women should be encouraged to attend an addiction unit that can manage their antenatal care and switch them to a safer alternative, such as prescribed methadone or buprenorphine. About 70% of exposed infants exhibit withdrawal symptoms, usually within 48 hours of birth, although they can be delayed for up to a week. Signs include extreme jitteriness, tachycardia, vomiting, diarrhoea and fever (see Table 4. Infants born to drug-addicted mothers may continue to show irritable or restless behaviour for a number of months after birth. Withdrawal can also occur if the mother has been on high doses of prescribed opiates for analgesia. Central nervous system Irritability and high-pitched cry Hyperactivity with reduced periods of sleep Tremors Increased tone Convulsions (rare) Poor feeding Vomiting Diarrhoea Sweating Fever Frequent yawning Snuffles and sneezing Tachycardia Gastrointestinal Other autonomic symptoms Management of neonatal abstinence syndrome Infants born to drug-addicted mothers should be carefully monitored for withdrawal symptoms. Breastfeeding should be encouraged, as the small amount of opiate excreted in breast milk may help alleviate symptoms. If severe signs of withdrawal are present, drug treatment is necessary and the first-line treatment is to give opiates such as oral morphine syrup. Various scoring systems are available; the most commonly used is the Finnegan score, which allocates a score to each of the symptoms shown in Table 4.
© 2025 Adrive Pharma, All Rights Reserved..