General Information about Benzoyl Peroxide
Benzoyl peroxide is also widely available, and you don't need a prescription to purchase it. It can be found in most drugstores, making it simply accessible to those that want it. It also offers an inexpensive option for these who could not be ready to afford expensive zits treatments.
In conclusion, Benzoyl peroxide is a extremely efficient and in style therapy for zits. Its antibacterial and anti-inflammatory properties make it a go-to solution for many skincare professionals. It is easy to use, has minimal side effects, and is available at an inexpensive worth. However, it's advisable to consult a dermatologist for customized treatment and to verify if benzoyl peroxide is appropriate for your pores and skin kind. With the right skincare routine, benzoyl peroxide might help you achieve clear and wholesome pores and skin.
Benzac, a model of 2.5% to 10% benzoyl peroxide gel, is specifically formulated to deal with acne. It is obtainable in completely different varieties, including topical lotions, gels, and washes, making it appropriate for different skin varieties and severity of pimples. The product is well-known and trusted by many skincare professionals, making it the go-to treatment for acne problems.
Unlike oral medications, benzoyl peroxide has very few unwanted effects. The most common aspect impact is skin dryness and irritation, which generally fades with steady use. It is advisable to start with a decrease focus of benzoyl peroxide and steadily increase it to reduce back the chance of irritation. If you experience any severe unwanted effects, it is best to seek the assistance of a dermatologist.
One of the explanations benzoyl peroxide is the preferred treatment for pimples is as a end result of it's extremely efficient. Research has proven that it might possibly remove acne-causing bacteria in as little as forty eight hours. It also prevents the formation of new zits lesions and reduces redness and inflammation associated with acne breakouts. With common use, it can also help in fading pimples scarring.
Moreover, benzoyl peroxide is comparatively straightforward to make use of. It can be integrated into one's day by day skincare routine with out much problem. For instance, Benzac has a variety of products that can be utilized as face washes or left on the pores and skin as overnight therapies. Its compatibility with different skincare merchandise is one more reason for its popularity. It can be used in combination with other pimples therapies, similar to retinoids and salicylic acid, for better and quicker outcomes.
Benzoyl peroxide is a topical medicine that belongs to the category of organic compounds called peroxides. It is broadly utilized in skincare products for its antibacterial and anti-inflammatory properties. When applied to the skin, it releases oxygen, killing the micro organism liable for inflicting pimples. It also helps to unclog pores by eradicating lifeless skin cells, excess oil, and different impurities.
Acne, a typical pores and skin situation that impacts tens of millions of individuals worldwide, may be distressing and confidence-shattering. It can manifest in various ways, from small blackheads and whiteheads to painful cysts and nodules. While there are heaps of therapies obtainable out there, one of the efficient and broadly used is benzoyl peroxide, sold beneath the brand name Benzac. Let's dive deeper into what benzoyl peroxide is and how it helps in treating acne.
Once traction alopecia is established and follicles have been lost acne 6 months after giving birth order line benzoyl, the hair loss becomes permanent. In infants and young children it is usually a habit akin to thumbsucking and nailbiting. It seems slightly more common in boys and usually resolves spontaneously or with minimal treatment. Parents who have not noticed hairpulling behaviour in their offspring may deny the diagnosis. In older age groups (adolescents and adults) trichotillo mania is seen predominantly in females, with women outnumber ing men by up to 7: 1, and evidence of some form of psychological or behavioural stress is often apparent [4]. The American Psychi atric Association classifies trichotillomania as an impulse control disorder, in which there is an irresistible desire to pull out the hair. Scalp electrodes or infusion [10] or forceps delivery in the neonate can result in trauma. Marks from such interventions need to be dis tinguished from aplasia cutis which can sometimes be the under lying diagnosis [12]. Interventions in adulthood, directly through scalp and brain surgery or indirectly though local embolization procedures, can result in scarring. There is an extensive psychiatric literature on tri chotillomania, but this may be biased because psychiatric help is likely to be sought only in those patients who accept that it is a selfinflicted problem. They may be broken, where trauma has snapped the shaft, or be tapered, where trauma is in the form of plucking. The scalp itself is usually clini cally normal except in the instances where the trauma is rubbing or scratching. In these instances there are often scalp symptoms and the problem may present primarily as a scalp dermatosis even if it is wholly artefactual. Rubbing can also lead to hair break age or interfere with the normal anagen cycle without specifically altering the hair shaft. Dermoscopy of the scalp may help differentiate between tri chotillomania and alopecia areata, where follicular orifices may appear as yellow dots [5]. Scalp histology varies according to the severity and duration of the hair plucking. Injured follicles may form only soft twisted hairs a process that has been described as a separate entity under the name of trichomalacia [7]. This results in a patch of hair loss, often in a bizarre or angular pattern, in which the hairs are twisted and broken at various distances from the clinically normal scalp. Older patients present with an area of scalp on which the hair has been reduced to coarse stubble uniformly, 2. It is unusual for hair to be lost completely within the affected area (in contrast with alopecia areata). Over time the extent of hair loss can vary, and hair growth may recover temporarily. Hair in sites other than the scalp can also be affected, such as eyelashes, eyebrows and beard. Exceptionally, the patient may pluck hair also, or only, from other regions of the body, such as the mons pubis and perianal region. A hairball (trichobezoar) is a rare accompaniment of trichotillo mania in those who also eat the plucked hair (trichophagia) [9]. Differential diagnosis the minor form in young children can be confused with ringworm or with alopecia areata. In ringworm, the texture of the infected hairs is abnormal and the scalp surface may be scaly. Alopecia areata may be difficult to exclude with certainty at the first exami nation, but the course of the condition usually establishes the cor rect diagnosis. Unlike alopecia areata, it is unusual for hair to be lost completely in trichotillomania and, in contrast with exclama tion mark hairs, the broken hairs of trichotillomania are firmly anchored in the scalp. Where doubt remains dermoscopy [5] or a skin biopsy will usually establish the correct diagnosis. However, there are reports of the coexistence of alopecia areata and tricho tillomania [4,10]. Syphilis Hair loss occurs in approximately 4% of cases of secondary syph ilis and may be the presenting feature [1,2]. The hair loss typi cally has a motheaten appearance but may be diffuse in nature [3]. Other features of secondary syphilis are present in most cases, particularly lymph node enlargement and hepatomegaly, but hair loss has been reported as the only sign of the disease [4]. Histological features include an increase in catagen and telo gen forms, and a peribulbar lymphocytic infiltrate, similar to the changes seen in alopecia areata [3]. Additional features in syphi lis include lymphocytic infiltration of the isthmus region, parab ulbar lymphoid aggregates and the presence of plasma cells within the infiltrate. The serpiginous nodulosquamous syphilide of tertiary syphilis may affect the scalp and the syphilitic gumma is a cause of scar ring alopecia. Management the establishment of a relationship between the physician and the patient, or with the parents of an affected child, is an important step in the management of trichotillomania. A confident diagnosis is essen tial, but this is not always easy and may require observation over time and sometimes a scalp biopsy. The habit tic in young children is often selflimiting, but input from a paediatric psychologist can be very helpful.
The face has a prematurely aged appearance with beaking of the nose skin care greenville sc buy discount benzoyl 20 gr line, and hair may be sparse and prematurely grey. Patients tend to develop early arteriosclerosis, diabetes, osteoporosis, hypertension and hypogonadism, and are at risk of cataracts and retinal degeneration. The median lifespan is in the midfifties with death usually the result of myocardial infarction or malignancy [13]. Exacerbation after exposure to sunlight is usual but not invariable, and light may also provoke bullae, bleeding and crusting of the lips. Extracutaneous features Patients with Bloom syndrome have a characteristic appearance. Patients have a narrow, slender, delicate facies with a relatively prominent nose and small jaw. The limbs tend to be long with large hands and feet, and there may be reduced subcutaneous fat. Other associated abnormalities include caféaulait patches, clinodactyly, syndactyly, congenital heart disease, annular pancreas and a highpitched voice, possibly due to the craniofacial anatomy and higharched palate. T and Bcell immunodeficiencies may occur, and IgA and IgM levels may be reduced predisposing to pneumonia, bronchiectasis and chronic lung disease. Gastrooesophageal reflux is also common and may lead to aspiration, contributing to the risk of chronic lung disease. Although the tubular elements of the testes function poorly, the androgensecreting portions are spared, thus permitting normal puberty [11]. Fertility in female patients appears reduced, although fullterm pregnancies have been reported [12]. Management Complications of Werner syndrome such as cardiovascular disease, diabetes and cataract are treated conventionally as and when they arise. Bloom syndrome Definition this syndrome is characterized by photosensitivity, telangiectatic facial erythema, proportionate pre and postnatal growth deficiency, distinctive facies, abnormal immune responses and a predisposition to malignancy [1,2,3]. Bloom syndrome occurs with greater frequency in Ashkenazi Jews, accounting for approximately onethird of all cases. A common ancestral mutation has been identified in most of these patients, with an estimated carrier frequency of 1%. Other founder mutations have also been identified in patients from other geographical regions [7,8]. Clinical features [1,3,911] Cutaneous features Telangiectatic erythema of the face develops during infancy or early childhood as red macules or plaques, which may simulate lupus erythematosus. Cancers of the types and sites seen in the general population arise frequently and unusually early, as do rare cancers of early childhood [10]. They are predominantly internal such as those of the upper and lower gastrointestinal tract, genitourinary cancers and haematological malignancies, but cutaneous malignancies are also more common with approximately 15% of patients in the Bloom Syndrome Registry having had skin cancer, with a mean age of 32 years [1,9]. Whilst some disorders are characterized by progeroid features, others involve cardiomyopathy, muscular dystrophy, peripheral neuropathy or lipodystrophy (see Table 79. Affected individuals usually die in childhood or teenage years due to cardiovascular causes. Management Early diagnosis of Bloom syndrome is important for awareness of the possible development of malignancies and for photoprotection. In the Ashkenazi Jewish population, where women have a one in 200 risk of having an affected child, targeted screening of the recurrent founder mutation may be indicated. Any symptoms suggestive of possible malignancy should prompt appropriate investigations. Aside from this, standard cancer treatments are recommended, as are treatments of associated diseases such as diabetes. Pathophysiology HutchinsonGilford progeria syndrome is an autosomal dominant condition with a birth prevalence estimated at one in 4 million [2]. This deletion interferes with the normal posttranslational modification of prelamin A leading to persistent farnesylation of progerin, which accumulates at the inner nuclear membrane causing increased cellular damage with age. Histopathologically, during the early sclerodermatous phase in the skin, thickening of the dermis with hypertrophic collagen bundles but a normal epidermis have been described [11], although changes may be nonspecific [12]. Later in life the epidermis may be thinned, the dermis replaced by fibrotic hyaline material, with a reduction of sweat glands and subcutaneous tissue [13]. Cutis laxa: autosomal dominant and autosomal recessive Definition Cutis laxa is a group of conditions in which the skin lacks elasticity leading to a loose, wrinkly and prematurely aged appearance. In addition to skin changes, these heterogeneous disorders are variably associated with connective tissue problems as a result of loss, disorganization or fragmentation of elastic tissues in other organs, notably the lungs, cardiovascular system, joints and gastrointestinal and genitourinary systems. Some forms are also associated with developmental delay and neuromuscular compromise. Management Management should be centred around monitoring disease progress, preventative care where possible, and treatment of complications as and when they arise [1,2]. Patients should have 612monthly growth, cardiovascular, neurological, musculoskeletal, dental, ear and eye assessments. Lipids, electrocardiogram, echocardiogram, carotid duplex scanning, hip Xrays and bone densiometry scans should also form part of annual care. Lowdose aspirin may be recommended in view of the increased risk of cardiovascular disease, and sun avoidance to limit cutaneous signs of increased ageing. Pathophysiology the formation of elastic fibres is a stepwise process and involves interplay between a number of different proteins. Microfibrils consisting of fibulin, fibrillin and various glycoproteins act as a scaffold for soluble tropoelastin monomers, which are then crosslinked by lysyl oxidase into an insoluble elastin core [4]. The head appears large for the face and scalp veins are prominent, made more noticeable due to alopecia which may be partial or total, and which may also affect the eyebrows and eyelashes. The eyes tend to be prominent, the lips are thin and may have surrounding cyanosis, and earlobes may be absent.
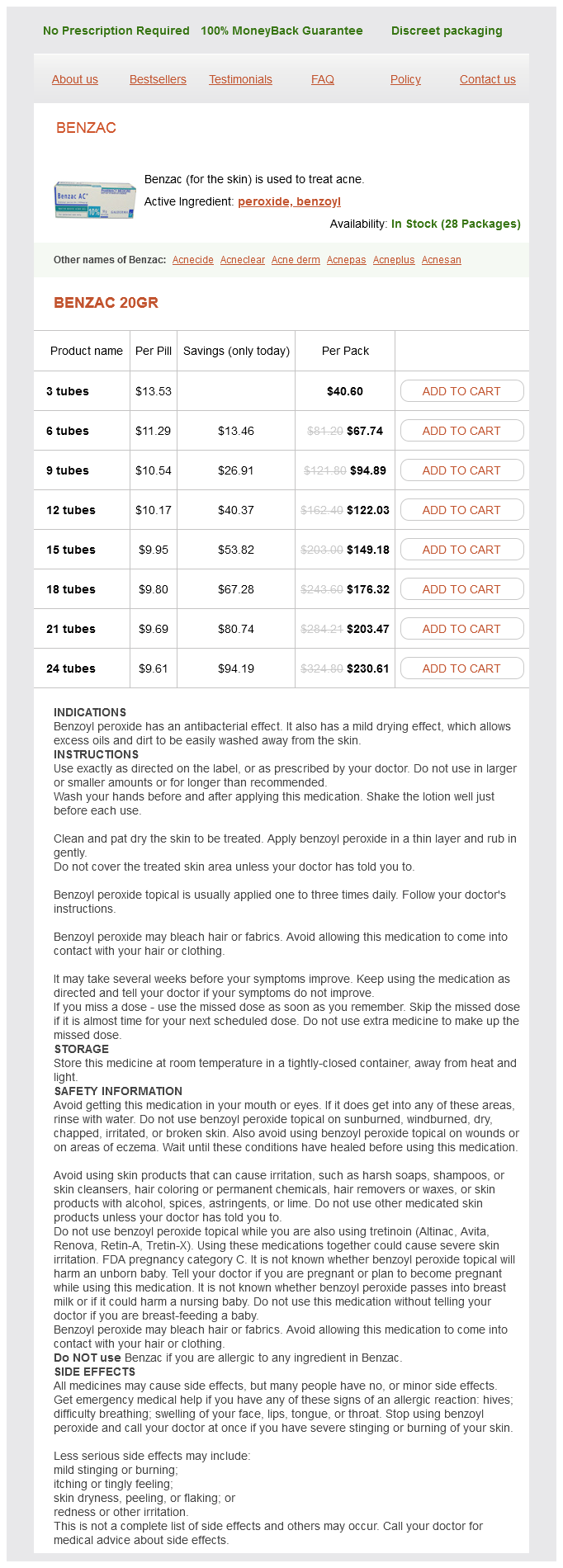
Benzoyl Peroxide Dosage and Price
Benzac 20gr
- 3 tubes - $40.60
- 6 tubes - $67.74
- 9 tubes - $94.89
- 12 tubes - $122.03
- 15 tubes - $149.18
- 18 tubes - $176.32
- 21 tubes - $203.47
- 24 tubes - $230.61
These include striate keratoderma with spastic paraplegia acne face chart discount benzoyl online visa, pes cavus and mental retardation in four brothers [1]; autosomal dominant punctate keratoderma and spastic paralysis [2]; autosomal dominant focal keratoderma with nail dystrophy and motor and sensory neuropathy [3]; and CharcotMarieTooth disease [4]. Atypical erythrokeratoderma with deafness has also been associated with peripheral neuropathy [5]. Clinical features Differential diagnosis As an example, acroosteolysis with keratoderma (BureauBarrière syndrome) [6,7] may show diffuse keratoderma with osteolysis in the forefoot area, polyneuropathy of the lower legs and painless ulcers of the feet. The disease is nonfamilial and often subsumed under the concept of neurotrophic ulcers [8]. Given the success of of etretinate, acitretine may be the treatment of choice [1]. The lesions of reactive arthritis are compact, heaped up and resemble the heads of nails (keratoderma blenorrhagica). Extensive hyperkeratotic eczema may be difficult to distinguish on clinical and histological grounds but marked itching may indicate eczema. The even orange hyperkeratosis of pityriasis rubra pilaris is associated with an acute follicular eruption in adults and by lesions on the knees and elbows in children. Keratoderma is also reported in association with acrocyanosis and livedo reticularis [12]. In lichen planus, warty lesions may be mistaken for viral warts; lichen planus and other lichenoid eruptions such as lichen nitidus may mimic punctate keratoderma [14]. Trichophytosis, especially resulting from Trichophyton rubrum, may be unilateral and lacking inflammatory signs. The tendency of secondary syphilis lesions to involve the palms is well known, and hyperkeratotic late syphilides may be warty or focal [15]. In immunocompromised patients, viral warts may be confluent on the palms or soles. Palmoplantar hyperkeratosis with myxoedema, improving with treatment, has been reported on several occasions [16,17]. In chronic lymphoedema, the skin overlying the lymphoedematous area first becomes diffusely thickened, and then develops into a velvety papillomatous surface, which is ultimately covered by large irregular warty projections (lymphostatic verrucosis; mossy foot) [1921]. Lymphoedematous keratoderma occurs most characteristically in filariasis, but may develop in the context of chronic lymphoedema of any origin. The dermis is oedematous with dilated lymphatics, conspicuous newvessel formation, some sclerosis and a variable infiltrate of inflammatory cells. Both the hyperkeratotic component and the lymphoedema improved in three cases given etretinate 0. Carcinogens, of which the best documented example is arsenic, may produce both keratoderma and internal malignancy [28,29]. One survey showed that palmar keratoses occur four to five times more frequently in patients with cancer than in controls [30]. An increased incidence of keratoses in patients with lung or bladder cancer has been debated [3133]. Keratoses associated with cancer are histologically distinct from arsenical keratoses [34]. Keratoderma may result from tegafur, glucan, lithium and halogenated weedkillers, and dioxin figure 65. Arsenicalinduced irregular warty keratoses, or more even glassy lesions, are still occasionally seen [40]. Agents used in cancer treatment commonly cause palmoplantar erythema (the handfoot syndrome) and may cause keratoderma [4143]. Cases have since been identified in several other countries, and a familial link to the Oudtshoorn cluster is evident in most. Pathophysiology It is an autosomal dominant disorder with variable penetrance and linkage to chromosome 8p22p23 has been reported in five South African and one German kindred [3]. The genetic alteration may have originated in a French immigrant in the late 1700s. A Norwegian family with four affected members did not show linkage to chromosome 8p22p23, suggesting genetic heterogeneity [6]. A frequent precipitant is cold dry weather and, although in South Africa it is most active in winter months, it may be perennial in temperate climates. Other triggers include febrile illness, surgery, stress and menstruation, and it improves in pregnancy and with age. The father of an affected toddler was unaffected but paternal aunts and other family members had similar palmoplantar eruptions and her paternal great great grandmother originated from Oudtshoorn [7], suggestive of partial penetrance. Episodes may be preceded by itch and hyperhidrosis and associated with pustulation. Palmoplantar erythema develops, and is followed by the evolution of painless superficial opaque dry blebs, which peel or can be pulled away, leaving a red base with intact markings. A second wave may begin at the centre of a lesion, resulting in gyrate and polycyclic annular erythema, which eventually resolves. Cycles repeat every few weeks and the palms and soles appear normal between attacks. Truncal lesions were reported in one patient [2], and facial involvement in another [8]. A similar phenotype affecting the palms, more active in summertime, was reported in Porokeratoses 65. Investigations Biopsy of the advancing edge of a lesion shows hyperplasia, spongiosis and, in the upper stratum spinosum, keratinocytes with pale cytoplasm, perinuclear vacuolization and pycnotic nuclei. In the abscence of a granular layer, the epidermis forms a parakeratotic wedge, which becomes sandwiched within the hyperkeratotic stratum corneum and is shed [2]. During regeneration, undifferentiated keratinocytes are not confined to the basal layer but appear in the lower half of the epidermis. Cytogenetic anomalies in fibroblasts, particularly chromosome 3, are also recorded [25].
© 2025 Adrive Pharma, All Rights Reserved..