General Information about Avodart
In conclusion, Avodart is an effective and well-tolerated medicine for the therapy of BPH. It has helped many males worldwide to enhance their symptoms and high quality of life. It is essential to do not forget that BPH is a progressive situation, and early therapy with medications like Avodart might help to stop the development of extreme problems. Therefore, it is needed to hunt medical recommendation should you expertise any urinary signs. With correct analysis and therapy, BPH may be successfully managed, allowing males to guide active and fulfilling lives.
BPH is a standard situation that affects males, particularly as they age. It is estimated that more than half of men over the age of 50 will expertise BPH. BPH is a non-cancerous situation, however it could cause varied urinary symptoms similar to frequent urination, a weak urine stream, and a sense of incomplete emptying of the bladder. These symptoms can considerably affect a man's high quality of life, and if left untreated, they'll lead to more critical issues similar to urinary tract infections and urinary retention.
Avodart, also known as Dutasteride, is a medicine commonly used to deal with Benign Prostatic Hyperplasia (BPH), a situation during which the prostate gland becomes enlarged. It is a prescription drug and has been clinically confirmed to be an efficient therapy for BPH in men. Avodart belongs to a category of drugs generally known as 5 alpha-reductase inhibitors which work by blocking the manufacturing of a male hormone known as DHT (dihydrotestosterone) which is liable for prostate gland enlargement.
Avodart has been in use since 2002 and has been broadly prescribed by doctors to treat BPH. The medication is taken orally within the form of a capsule, and it really works by inhibiting the activity of the enzyme 5 alpha-reductase, which converts testosterone to DHT. By blocking the manufacturing of DHT, Avodart effectively reduces the scale of the prostate gland, thus improving urinary signs and move price. It also helps to reduce back the risk of acute urinary retention and the need for surgery associated to BPH.
However, like any other treatment, Avodart also has its share of potential unwanted side effects. The most common reported side effects of Avodart embrace sexual dysfunction, corresponding to decreased libido, erectile dysfunction, and decreased semen quantity. These side effects are generally gentle and have a tendency to resolve once the treatment is stopped. In uncommon circumstances, Avodart can also trigger allergic reactions, breast enlargement or tenderness, and despair.
It is crucial to hunt medical advice earlier than starting to take Avodart. The treatment is not suitable for everybody, and individuals with sure medical situations, such as liver disease, mustn't take it. It can even interact with different drugs, so it's crucial to inform your doctor of all medicines you might be at present taking.
Avodart has additionally been just lately accredited by the FDA to be used together with one other medicine, tamsulosin, for the remedy of BPH. This combination has been proven to be more practical in bettering urinary signs than both treatment alone. Tamsulosin is an alpha-blocker that helps to relax the muscles within the prostate and bladder, making it simpler to urinate.
One of the main advantages of Avodart over other BPH medications is its long period of motion. While different BPH medications need to be taken regularly, Avodart solely must be taken once a day, making it extra handy for sufferers. Studies have additionally shown that Avodart supplies extended relief of symptoms, with some sufferers experiencing improvement for as a lot as four years.
Analysis of therapeutic effect for schizophrenia with risperidone and perphenazine symptoms jaw bone cancer avodart 0.5 mg purchase amex. A comparative study between perphenazine and risperidone on the effect on the life quality of the patients with schizophrenia. Olanzapine versus haloperidol in randomized trials of first-episode patients with schizophrenia. Comparitive double-blind trial of the efficacy of risperidone, haloperidol and levomepromazine (methotrimeprazine) in patients with an acute exacerbation of schizophrenia presenting psychotic anxiety symptoms. Autonomic effects of clozapine in schizophrenia: comparison with placebo and fluphenazine. Comparative clinic analysis of risperidone and haloperidol for treatment of schizophrenic negative symptoms. List of Companion Studies A total of 146 articles were companions to the included studies. Impact of second-generation antipsychotics and perphenazine on depressive symptoms in a randomized trial of treatment for chronic schizophrenia. Intramuscular aripiprazole or haloperidol and transition to oral therapy in patients with agitation associated with schizophrenia: sub-analysis of a double-blind study. The relationship of clozapine and haloperidol treatment response to prefrontal, hippocampal, and caudate brain volumes. Acute weight gain, gender, and therapeutic response to antipsychotics in the treatment of patients with schizophrenia. Serum glucose and lipid changes during the course of clozapine treatment: the effect of concurrent betaadrenergic antagonist treatment. Neurocognitive effects of clozapine, olanzapine, risperidone, and haloperidol in patients with chronic schizophrenia or schizoaffective disorder. Contrasting the effects of haloperidol and olanzapine on attention and working memory in schizophrenia: a double-blind flexible dose study [dissertation] 2004. Risperidone in combination with mood stabilizers: a 10-week continuation phase study in bipolar I disorder. The effect of clozapine on plasma norepinephrine: relationship to clinical efficacy. The comparative efficacy and long-term effect of clozapine treatment on neuropsychological test performance. Efficacy and tolerability of quetiapine in poorly responsive, chronic schizophrenia. A post hoc analysis of the impact on hostility and agitation of quetiapine and haloperidol among patients with schizophrenia. Effects of risperidone in tardive dyskinesia: an analysis of the Canadian multicenter risperidone study. Efficacy of ziprasidone against hostility in schizophrenia: post hoc analysis of randomized, open-label study data. The acute and long-term effect of olanzapine compared with placebo and haloperidol on serum prolactin concentrations. Interleukin-12 plasma levels in drug-naive patients with a first episode of psychosis: effects of antipsychotic drugs. Neurocognitive effectiveness of haloperidol, risperidone, and olanzapine in firstepisode psychosis: a randomized, controlled 1-year followup comparison. Effect of antipsychotic drugs on brain morphometry: a randomized controlled one-year followup study of haloperidol, risperidone and olanzapine. Relapse prevention and remission attainment in firstepisode non-affective psychosis. A randomized, controlled 1-year followup comparison of haloperidol, risperidone and olanzapine. Antipsychotic-induced weight gain and therapeutic response: a differential association. Double-blind, randomized comparison of olanzapine versus fluphenazine in the long-term treatment of schizophrenia. A singleblind, randomized trial comparing quetiapine and haloperidol in the treatment of tardive dyskinesia. Differential effect of quetiapine on depressive symptoms in patients with partially responsive schizophrenia. Risperidone versus haloperidol for facial affect recognition in schizophrenia: findings from a randomized study. Maintenance treatment with risperidone or low-dose haloperidol in first-episode schizophrenia: 1-year results of a randomized controlled trial within the German Research Network on Schizophrenia. Supplementing clinic-based skills training with manual-based community support sessions: effects on social adjustment of patients with schizophrenia. Superior efficacy of olanzapine over haloperidol: analysis of patients with schizophrenia from a multicenter international trial. First episode schizophrenia-related psychosis and substance use disorders: acute response to olanzapine and haloperidol. The neurocognitive effects of low-dose haloperidol: a two-year comparison with risperidone. Functional outcomes in schizophrenia: a comparison of olanzapine and haloperidol in a European sample.
Interestingly medications with dextromethorphan cheap avodart 0.5 mg overnight delivery, choreiform movements in tardive dyskinesia are worsened by anticholinergics (Greil et al. Patients who develop a depressive syndrome typically experience a worsening of symptoms (Sachdev 1989), whereas during mania there may be a partial remission (de Potter et al. Etiology Although the vast majority of cases of tardive dyskinesia occur secondary to treatment with antipsychotics, cases have also been reported with other dopamine blockers, such as metoclopramide (Sewell and Jeste 1992; Sewell et al. Given that all of the drugs capable of causing tardive dyskinesia have one thing in common, namely a blockade of post-synaptic dopamine receptors, and given that the risk of tardive dyskinesia increases with higher doses (Morganstern and Glazer 1993) and a longer duration of treatment (Glazer et al. Further support for a disturbance in dopamine transmission is provided by the response to anticholinergics in tardive dyskinesia. Dopaminergic and cholinergic systems exist in a balance in the basal ganglia, such that an increase in dopaminergic tone may be mimicked by a reduction in cholinergic tone and vice versa. Given this one would predict that, in patients with tardive dyskinesia, a reduction in cholinergic tone, as might occur with the administration of an anticholinergic medication, would increase the abnormal movements, and this is generally what happens (Klawans and Rubovits 1974). As attractive as this dopamine theory is, it does not account for several important findings. First, the fact that acute antipsychotic-induced parkinsonism can co-exist with Course the course of tardive dyskinesia has been most thoroughly studied with reference to the choreiform type. In situations in which the antipsychotic is continued at a constant dose, there is a gradual worsening of symptoms; although in most cases the severity eventually reaches and stays at a plateau, in a minority one sees a relentless progression (Gardos et al. If the antipsychotic is discontinued there is typically a pronounced worsening of symptoms, which is followed, however, over the succeeding weeks or months, by at least some diminution of symptoms, after which one of two eventualities may ensue (Glazer et al. Second, some cases of the dystonic subtype of tardive dyskinesia may, as noted below, be relieved by, rather than worsened by, anticholinergic agents. Unfortunately for the theory, however, tardive dyskinesia does in fact emerge while patients continue at the same dose, a fact strongly suggesting that some other process, in addition perhaps to a progressive up-regulation, is at work. This last theory is of some interest given the evidence, noted below, for the treatment efficacy of vitamin E, an antioxidant. When tardive dyskinesia does first appear, a decision must be made as to whether ongoing treatment with a neuroleptic is required, carefully weighing the risk of worsening dyskinesia against the risk of relapse. In the case of schizophrenia, the balance often tips towards continuing neuroleptic treatment. If treatment is continued, efforts, if not already in place, should be made to keep the dose as low as possible, consistent with adequate symptomatic control. In cases due to treatment with a first-generation antipsychotic, consideration should be given to switching to a second-generation agent; with such a switch, adequate symptom control is maintained or improved and the risk of worsening tardive dyskinesia with further treatment is lessened. In cases in which treatment cannot be discontinued, or in cases in which discontinuation is possible but symptoms fail to go into remission, various medical treatments may be considered, including vitamin E, vitamin B6, melatonin, branched chain amino acids, piracetam, and dopamine depletors, such as tetrabenazine, alpha-methyldopa or reserpine. The overall differential diagnoses of chorea, dystonia, akathisia, and tics are discussed in Sections 3. Schizophrenia may at times be characterized by choreiform movements, as pointed out by Kraepelin in the early part of the twentieth century (Kraepelin 1971) and confirmed by subsequent investigators (Farran-Ridge 1926; Mettler and Crandall 1959; Owens et al. Both dystonia and akathisia may occur as acute extrapyramidal side-effects of antipsychotics but are readily distinguished from tardive dystonia or tardive akathisia by their p 22. From a pharmacologic viewpoint branched chain amino acids constitute an interesting option (Richardson et al. Administration of a combination of valine, isoleucine, and leucine (given in a ratio of 3:3:4 at a dose of 222 mg/kg three times daily) is followed by a fall in the plasma levels of the aromatic amino acids tyrosine and tryptophan, with presumably a fall in central nervous system levels of dopamine and serotonin, and it is this change that presumably accounts for the improvement in the tardive dyskinesia. Piracetam (not available in the United States), in a dose of 4800 mg/day, was recently found to be effective (Libov et al. Of these options, the vitamins and melatonin are the most benign, and one of these should probably be tried first; vitamin E has by far the most support and is a reasonable starting point. In some cases combination treatment with two or more of these agents may be appropriate. Branched chain amino acid treatment is also generally benign, but should not be used in diabetics. The dopamine depleters, given their unfavorable side-effect profile, should generally be held in reserve. Botulinum toxin may be considered in cases in which the abnormal movement is well-localized, as may be seen with certain choreiform movements or, more especially, dystonia. In the case of tardive dystonia, anecdotal reports support treatment with high-dose anticholinergic agents (Burke et al. However, the occurrence of this supersensitivity psychosis in patients treated with antipsychotics who have never had symptoms of schizophrenia, or any other psychosis, clearly indicates that the syndrome, although rare, does exist (Moore 1986). Clinical features After a year or more of treatment with an antipsychotic, the syndrome emerges. This emergence may be fairly abrupt if the antipsychotic is discontinued or there is a rapid dose reduction; in other cases a more gradual onset may occur, for example when the dose of the antipsychotic is held constant or only gradually and modestly decreased. Course Although the course has not been well-studied, it appears that, in cases in which the antipsychotic is discontinued, symptoms very gradually lessen; the percentage of cases that go on to full remission or a stable chronicity is not known. Etiology Although the etiology is not known, it is speculated that with chronic treatment with antipsychotics there is an up-regulation of post-synaptic dopamine receptors within the limbic system leading to a chronic hyperdopaminergic state. Of note, cases have also been described secondary to chronic treatment with the dopamine-blocker metoclopramide (Lu et al. Differential diagnosis the diagnosis should only be entertained in patients who have been treated chronically with an antipsychotic or other dopamine blocker.
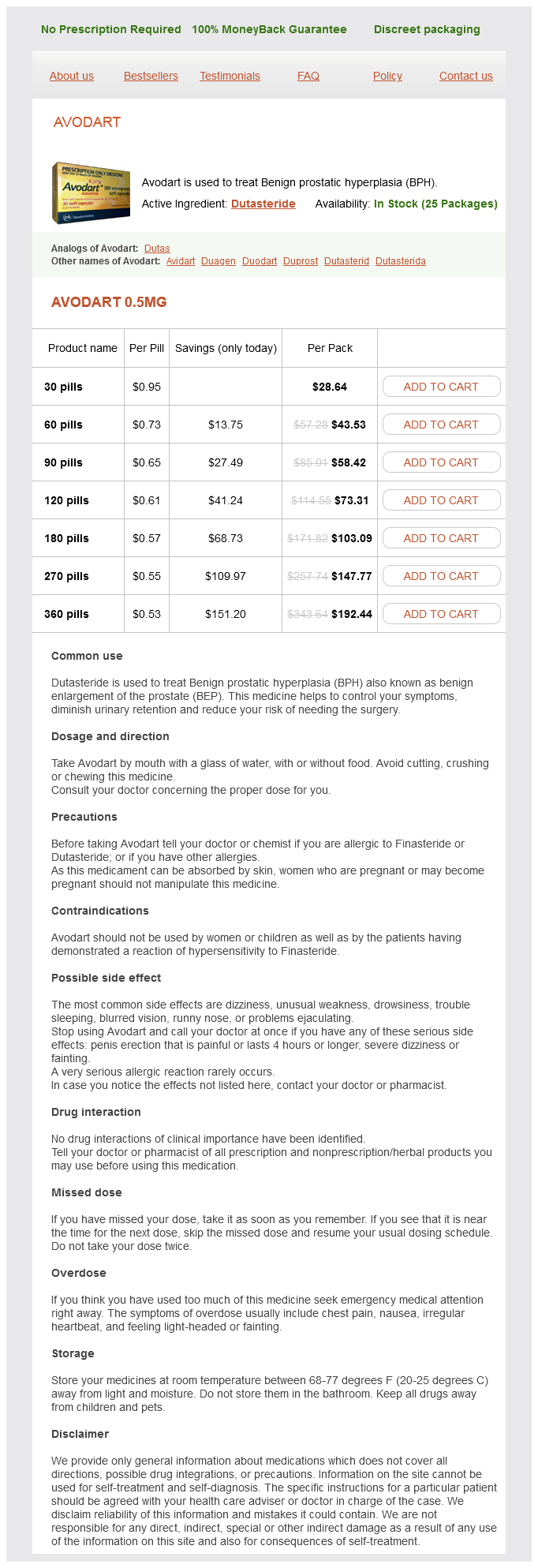
Avodart Dosage and Price
Avodart 0.5mg
- 30 pills - $28.64
- 60 pills - $43.53
- 90 pills - $58.42
- 120 pills - $73.31
- 180 pills - $103.09
- 270 pills - $147.77
- 360 pills - $192.44
About 99% of all conceptuses with chromosomal abnormalities die prenatally symptoms crohns disease order cheapest avodart and avodart, including almost all cases of monosomy X, polyploidy, and autosomal trisomy; one-half of fetuses with trisomy 21 die prenatally. Forty percent of liveborn Down syndrome children die by the end of the first year of life. Nondisjunction appears to be nonrandom because women who have had a chromosomally unbalanced fetus are more likely to have another aneuploid fetus if they miscarry again than women whose first miscarried fetus was chromosomally normal. The risk of recurrence after one affected child with a standard trisomy is about 1% for a baby with some form of trisomy (trisomy 21 would be the most common). Approximately 25% of liveborn infants with chromosomal abnormalities have autosomal trisomy, and approximately 40% have a structural chromosomal defect. Those with balanced structural chromosomal defects are phenotypically normal but have some 15% fewer liveborn offspring than their chromosomally normal siblings. The phenotypic expression of chromosome abnormalities can be readily observed in the fetus. The pathologic changes can be recognized and some pathologic markers for specific chromosome abnormalities may be apparent in early fetal life such as cystic and calcified Hassal corpuscles in trisomy 21, gelatinous multivalvular disease in trisomy 18, partial hydatidiform mole of the placenta in triploidy, and cystic hygromas in Turner (45,X) syndrome. The incidence and types of chromosome abnormalities in spontaneous abortions are listed in Table 6. Disturbance of growth results in 1x intrauterine growth retardation or a small-for-gestational-age infant. Aneuploidy has more or less severely deleterious develUp to 19 2024 2529 3034 3539 opmental effects on gonads. Turner syndrome is associated with Maternal age gonadal dysgenesis of late fetal ovarian degeneration, and Kline- 6. A mild malformation is an anomaly of morphogensis and should be viewed as a reduced expression of a major anomaly. A list of the more common mild malformations seen in chromosomal defects is shown in Table 6. The pathologic examination in chromosomal defects includes procedures mentioned in Table 6. Cystic and calcified Hassal corpuscles recognized as well as gelatinous valvular tissue in the heart. This involves all valves (multivalvular) and represents persistence of early fetal valvular development. Dermatoglyphics of Down syndrome (trisomy 21) (right) compared with the normal (left). Middle phalanx of fifth finger is hypoplastic; a proximal epiphysis is present on the second and distal epiphysis on the first finger (arrows). General features of abnormalities observed in trisomy 21 include intrauterine growth retardation; diminished sucking and swallowing reflexes; 6. There is a short anteroposterior diameter, an open operculum, and a hypoplastic superior temporal gyrus. A small percentage of translocation cases have an isochromosome for the long arm of chromosome 21 t(21q:21q). The risk of a liveborn infant with Down syndrome increases with the age of the mother. If the mother carries a 14:21 translocation, recurrence risks are 10% and if the father carries such a translocation, the risks are 2%. This male infant shows the typical phenotype of trisomy 18 including micrognathia, low-set ears, slender bridge of the nose, short sternum, narrow pelvis, clenched fists with the index finger overlapping the 3rd finger, and rocker-bottom feet. Microscopic section of liver showing giant cell transformation of hepatocytes and cholestasis not infrequently seen in trisomy 18. Cri du chat syndrome: hypertelorism, oval face, antimongoloid slant of the eyes and large ears. Microscopic appearance of a pancreatic islet; cytomegaly of the cells that are somatostatin positive by immunoperoxidase staining. Type 1: 85%, extra haploid set of chromosomes of paternal origin, normal fetal growth, microcephaly, and a partial hydatidiform mole. Type 2: 15%, extra haploid set of maternal origin, severe intrauterine growth retardation, relative macrocephaly, and a small noncystic placenta. There is an increased carrying angle at the elbows and shield-shaped chest, gonadal dysgenesis with absent or delayed and scanty menstruation and infertility develop later. The chorionic villi are large, with scalloping at the margins, trophoblastic inclusion, and an edematous stroma. It is the most common sex-chromosome abnormality in females and affects an estimated 3% of all females conceived. More than half of all patients with Turner syndrome have a mosaic chromosomal complement. The use of fluorescence in situ hybridization increases the detected prevalence from 34% with conventional cytogenetic techniques to 60%, and the use of reverse transcriptionpolymerase chain reaction assays as well, further increases the detected prevalence to 74%. Mosaicism with a normal cell line in the fetal membranes may be necessary for adequate placental function and fetal survival. Typical findings include thickening of the nuchal fold, cystic hygroma, renal (horseshoe kidney), and left-sided cardiac abnormalities (coarctation of the aorta). Some progress to term uneventfully but it may be associated with intrauterine fetal death, intrauterine growth retardation, and prenatal mortality.
© 2025 Adrive Pharma, All Rights Reserved..