General Information about Atomoxetine
While Strattera is generally well-tolerated, like all medication, it may cause side effects in some individuals. The most typical side effects include nausea, dry mouth, decreased urge for food, and abdomen ache. In some cases, individuals may also experience dizziness, fatigue, or mood modifications. It is essential to discuss any unwanted side effects with a health care provider to discover out if any changes have to be made to the dosage or if an alternate medicine should be considered.
Unlike other ADHD medications, Strattera does not have the potential for abuse or addiction. This makes it a safer choice for people who have a historical past of substance abuse or who are vulnerable to growing substance use problems.
There is a big amount of research that helps the effectiveness of Strattera in treating ADHD signs. In a examine printed in the Journal of the American Academy of Child and Adolescent Psychiatry, it was discovered that Strattera reduced ADHD symptoms in youngsters aged 6-12 years by 33%. It has also been discovered to be efficient in lowering symptoms in adults with ADHD.
Strattera works by inhibiting the reuptake of the neurotransmitter norepinephrine. Norepinephrine is a chemical that plays a job in regulating attention and habits. By increasing the degrees of norepinephrine, Strattera helps improve consideration and management impulsiveness and hyperactivity.
In conclusion, Strattera (atomoxetine) is an effective and secure treatment for managing symptoms of ADHD in each youngsters and adults. It provides an different to stimulant medicines and has a low threat of habit or abuse. However, like several treatment, it's important to observe the prescribed dosage and talk about any issues or unwanted effects with a health care provider. With proper use and adherence to therapy, Strattera might help individuals with ADHD improve their focus, attention, and total high quality of life.
Strattera is available in capsule type and is often taken a couple of times a day, depending on the individual's needs. It is essential to comply with the prescribed dosage and to not abruptly stop taking the medicine without consulting a physician. It may take several weeks for Strattera to work successfully, and it isn't a treatment for ADHD. It is supposed to be used as a part of a comprehensive therapy plan that may also include remedy and habits modifications.
Atomoxetine, also recognized by its model name Strattera, is a medication used to treat attention-deficit/hyperactivity dysfunction (ADHD). It is a non-stimulant treatment, in distinction to different commonly used ADHD drugs corresponding to Ritalin or Adderall. Strattera has been approved by the United States Food and Drug Administration (FDA) to be used in both youngsters and adults.
Another advantage of Strattera is that it has a long-lasting impact. This signifies that it does not need to be taken multiple occasions all through the day, making it a convenient choice for individuals managing their ADHD signs while at work or college.
ADHD is a neurodevelopmental disorder that is characterized by symptoms such as hyperactivity, impulsivity, and problem with attention and focus. It is estimated that about 5% of children and a pair of.5% of adults have ADHD worldwide. While the precise explanation for ADHD is not fully understood, it's believed to be a mix of genetic, environmental, and neurobiological components.
As progress is made with the hand drill medications not to take after gastric bypass generic atomoxetine 40 mg otc, gradually reduce pressure to avoid inadvertent "plunging" into the brain parenchyma. The operator will know when penetration through both the outer and inner tables of the skull has been accomplished once resistance against the drill is no longer felt. After skull penetration has been accomplished, remove the round piece of bone that has been cored out (with the diameter of the drill) and place it in saline. In many cases, epidural blood and clots under pressure will extrude from the site on full penetration of the skull. However, insertion of a suction catheter into the trephinated space may be necessary for full evacuation of clotted material. If easily identified, the bleeding artery (usually the middle meningeal artery) may be clamped. In a significant minority of patients, false localizing signs may lead the clinician to suspect a hematoma on the wrong side. Thus, if no improvement is noted with trephination on the side of the suspected hematoma, the procedure may be repeated on the opposite side. However, in all cases the delay in definitive neurosurgical care caused by attempts at trephination must be weighed against the possible benefits of the procedure. Moreover, trephination should ideally be performed after consultation with the accepting neurosurgeon. A slit valve may be used in the far end of the distal tubing instead of a more proximally placed valve, as shown. An estimated 30,000 intracranial shunts are placed in the united States every year. Intracranial shunts have a high rate of failure and represent a disproportionately high number of hospital readmissions. The essential elements of the shunt system include a proximal and a distal catheter, a valve, and a reservoir. The valve allows unidirectional flow, incorporates a pumping chamber, and regulates the pressure at which flow will occur across it. The proximal valve allows flow from the ventricles to the reservoir, whereas the distal valve allows flow from the reservoir to the distal catheter. Many different types of shunt systems, incorporating a variety of designs, are available. Some have unique characteristics, such as a double dome, whereas in others, valves are absent altogether. In most cases the reservoir allows for measurement of pressure, testing for patency, fluid sampling, and injection of medication or contrast material. In rare cases, other equipment is incorporated into the shunt system for specific purposes, including an on-off switch, a telemetric pressure sensor, and an anti-siphon device. Other types of shunts include ventriculovenous, ventriculoatrial, ventriculopleural, and lumboperitoneal. Ventricular catheters can be either straight or angled, with the latter having the option of a reservoir component attachment. Valves come in four different types (ball, diaphragm, miter, slit), each with unique flow characteristics. Identifying the type of shunt in place is often difficult unless the patient or caretaker has the information available. Moreover, the skin overlying the subcutaneous component of the shunt in the temporal regions can scar, thus rendering palpation of the shunt type impossible. The proximal inlet tube and silicone base are placed in the bur hole so that only the reservoir (silicon dome) protrudes above the skull. Peritoneal shunts may be associated with infection (peritonitis) or mechanical obstruction. Some evidence suggests that delayed hypersensitivity to the shunt material is also an occasional cause of obstruction. Postoperatively, following shunt placement, the ventricles usually begin to diminish in size within a week in patients with high-pressure hydrocephalus, so continued enlargement suggests (but does not confirm) shunt malfunction. This is a relatively rare cause of shunt failure and is estimated to occur in approximately 3. This reflects a variety of factors, including the ability to adhere to shunt surfaces, as well as production of mucoid substances that protect the bacteria from host defenses. The diagnosis may be obvious in patients with variable systematic signs, wound infection, meningitis, peritonitis, or septicemia. In children, lethargy, poor feeding, vomiting, ataxia, decreased or increased activity level, fussiness, fever and diaphoresis, as well as bulging fontanelles can all be indications of shunt malfunction. Fever, particularly within the first 6 months after surgery, is strongly associated with shunt infection. Symptoms of shunt malfunction may be difficult to interpret, particularly if the symptoms are atypical or nonspecific or if they occur in young children. Clinical evaluation of a child may not always be diagnostic of a shunt malfunction. Shunt Infection: Treatment and Prevention Of all the potential complications associated with shunting procedures, infection is the most notorious and occurs in 2% to 10% of cases. Other risk factors associated with shunt infection include perioperative infection and dental or urologic instrumentation.
Follow-up of 118 men with flat lesions showed a benign clinical course and regression in 90% of the cases in 5 years medicine nobel prize 2015 purchase 25 mg atomoxetine visa, usually within 12 months. In non-Western countries, up to 40% of patients present with inguinal lymph node metastasis and 10% with disseminated disease. In areas of high frequency, the majority of tumors are initially dignosed as invasive tumors whereas in regions of low incidence, most cases are diagnosed as in situ lesions. Invasive squamous cell carcinoma Squamous cell carcinoma arises on the mucosal surface of the penis extending from the preputial orifice to the urethral meatus, comprising the inner surface of the foreskin, coronal sulcus and glans. Distal urethral tumors, morphologically similar to some penile tumors, are not discussed in this text. In the fresh state or after fixation there may be a contrast between the white color of the tumor and the reddish, darker penile tissue. When these features predominate, there is a morphological justification for separation of the neoplasm as a special subtype of squamous cell carcinoma. Genital intraepithelial neoplasia and squamous carcinoma 499 Subtypes of squamous cell carcinoma Table 12. Lauren ackerman in 1948 in the buccal mucosa, verrucous carcinoma continues to pose diagnostic problems with other verruciform tumors sharing some of its characteristics. We have proposed a classification of verruciform neoplasms that helps to differentiate verrucous carcinoma from other similar lesions. Most tumors are unicentric but multicentric cases or association with other subtypes such as the pseudohyperplastic variant has been observed. Grossly, it is an exophytic papillomatous tumor with some variation in the configuration of the papillae, from multinodular with cobblestone morphology to filiform with a spiky appearance. Verrucous carcinoma is superficial, rarely penetrating beyond lamina propria or superficial dartos or corpus spongiosum. Histological features Microscopically, the tumor is diffusely well differentiated, resembling nomal squamous epithelium except for the presence of occasional atypical nuclei in the basal or parabasal layers. Features include papillomatosis, hyper- to orthokeratosis, acanthosis and a broad-based interface between the tumor and stroma, the latter considered pathognomonic for this tumor. Lichen sclerosus is a further frequently found associated condition and may be pathogenetically related to verrucous carcinoma. Condylomatous (warty) carcinoma Clinical features Condylomatous carcinoma is a slowly growing, verruciform low- to intermediate-grade hpV-related tumor, grossly similar to giant condyloma but with malignant histology and potential for nodal metastasis. Unlike benign condyloma, koilocytosis is not restricted to the surface epithelial cells but is also present in deep invasive portions of the tumor. Deeply invasive, high-grade condylomatous carcinoma may be associated with inguinal nodal metastasis. Koilocytosis, condylomatous papillae and jagged irregular boundaries between tumor and stroma are present in warty but not in verrucous carcinomas. Giant condylomas are broadly based noninvasive tumors with surface koilocytosis (see Table 12. Microscopically, the appearance is that of a well-differentiated papillary squamous neoplasm. Differentiating features from verrucous and condylomatous carcinoma are based on the heterogeneity of the papillae, the lack of koilocytosis and the jagged irregular interface between tumor and stroma. Low-grade squamous intraepithelial lesion and lichen sclerosus are frequently associated with papillary carcinoma. Occasional palisading at the nest periphery may be noted but it is usually not as prominent as is seen in basal cell carcinoma of the skin. Unusual morphological features of basaloid carcinomas In accordance with their common hpV etiology, some tumors show mixed basaloidcondylomatous features. Unlike other penile papillary tumors, the papillae are entirely composed of small cells simulating a transitional urothelial carcinoma. Sarcomatoid carcinoma (carcinoma with heterologous differentiation, metaplastic carcinoma) Clinical Features Sarcomatoid carcinoma is an aggressive penile neoplasm composed predominantly of spindled cells. It may arise de novo, follow a recurrence of usual squamous cell carcinoma or develop after irradiation therapy of a verrucous carcinoma. It accounts for about 14% of all penile carcinomas and preferentially involves the glans penis although the foreskin may also be affected. Grossly, it presents as a bulky 510-cm ulcerated or rounded polypoid mass, which on sectioning shows almost invariably deep invasion into the corpus cavernosum. Histological features Microscopically, there are variable proportions of squamous and spindled cell carcinoma but the latter usually predominates. Immunohistochemistry is essential for tumors with little or no epithelial component and for small biopsy specimens. In our experience, cytokeratin 34betae12 and p63 appear to be the more specific and sensitive markers to categorize these tumors as epithelial. Smooth muscle actin can be focally positive; however, desmin, muscle-specific actin, myogenin and S-100 are negative. It is often multicentric and the second or third independent lesion is sometimes verrucous. We have observed similar cutaneous tumors in association with severe solar elastosis or in scars after burns. In a series of 10 cases, recurrence was noted in the glans of one patient who was circumcised for a multicentric carcinoma of the foreskin 2 years after diagnosis. Histological features Characteristic microscopic features are keratinizing nests of squamous cells with minimal atypia surrounded by a reactive stroma. It is a deeply penetrating, albeit low-grade squamous cell carcinoma which, because of its burrowing growth pattern, was designated epithelioma cuniculatum by ayrd in 1954. Grossly, the tumor is whitegray, exoendophytic and papillomatous with a cobblestone or spiky appearance.
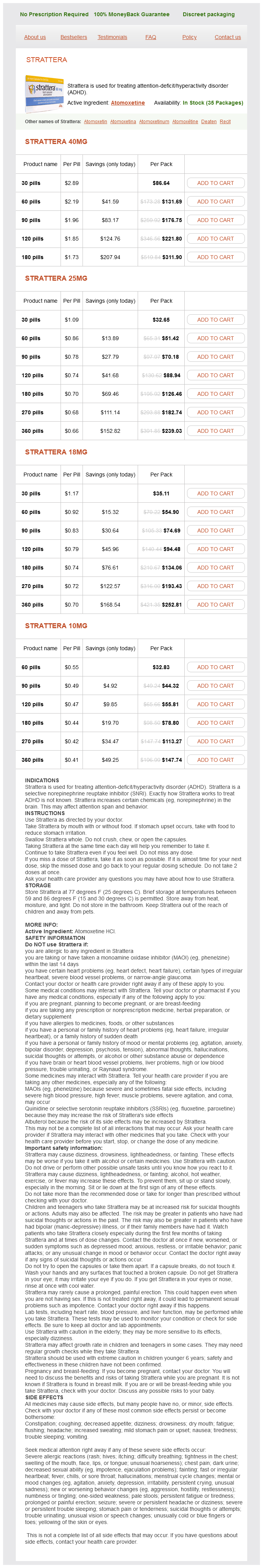
Atomoxetine Dosage and Price
Strattera 40mg
- 30 pills - $86.64
- 60 pills - $131.69
- 90 pills - $176.75
- 120 pills - $221.80
- 180 pills - $311.90
Strattera 25mg
- 30 pills - $32.65
- 60 pills - $51.42
- 90 pills - $70.18
- 120 pills - $88.94
- 180 pills - $126.46
- 270 pills - $182.74
- 360 pills - $239.03
Strattera 18mg
- 30 pills - $35.11
- 60 pills - $54.90
- 90 pills - $74.69
- 120 pills - $94.48
- 180 pills - $134.06
- 270 pills - $193.43
- 360 pills - $252.81
Strattera 10mg
- 60 pills - $32.83
- 90 pills - $44.32
- 120 pills - $55.81
- 180 pills - $78.80
- 270 pills - $113.27
- 360 pills - $147.74
C symptoms flu order generic atomoxetine pills, Inferior surface of heart showing vein graft anastomosis with posterior descending artery. Note metallic ring marker placed at origin of vein graft by surgeons for use in subsequent heart catheterizations. B, "Angio" display better delineates graft from origin at the left subclavian artery to its two anastomoses. Unusual variation with a vein graft arising from the descending aorta, passing over the left pulmonary artery, and then anastomosing with an obtuse marginal branch of the circumflex artery. The human heart has three systems of veins: the left ventricular, the right ventricular, and the thebesian veins. The left ventricular system drains most of the left ventricular venous blood and is formed by the anterior interventricular vein, the left marginal vein, the middle cardiac vein, and the right marginal vein. The great cardiac vein follows in continuity with the coronary sinus that ends in the right atrium. The posterior ventricular vein, or middle cardiac vein, that runs in the posterior interventricular sulcus may drain into the right atrium or into the coronary sinus. The right ventricle veins are known as the anterior cardiac veins and are two to four long veins crossing the anterior surface of the right ventricle and draining directly into the right atrium. The small thebesian veins drain directly into the right atrium and right ventricle. The coronary sinus is becoming increasingly important in the clinical practice of medicine, as it is a commonly used location for the placement of pacemaker and other electrophysiologic leads. During angiography, a catheter is directed into the right atrium and then into the coronary sinus. The tip of the lead may then be placed in the great cardiac vein or the middle cardiac vein. In addition, when an anomaly of a left-sided inferior vena cava occurs, this most commonly empties into the coronary sinus. Anterior interventricular vein and other small veins emptying into the great cardiac vein. The great cardiac vein running in the left atrioventricular groove along with the circumflex coronary artery. View from the bottom of the heart showing drainage of the right marginal, middle cardiac vein, left marginal, and great cardiac vein into the coronary sinus. Subclavian Artery Vertebral artery Internal thoracic artery (internal mammary artery) Thyrocervical trunk Costocervical trunk Dorsal scapular artery Inferior Thyroid Artery. Vertebral Artery this artery is described in the head and neck section (Chapter 2). Internal Thoracic Artery (Internal Mammary Artery) this artery arises within 2 cm of the origin of the subclavian artery. It courses forward and downward behind the cartilages of the upper ribs and divides into the musculophrenic and superior epigastric arteries at the level of the sixth intercostal space. Suprascapular Artery (May be a branch of the Subclavian or Internal Thoracic Artery. Thyrocervical Trunk the thyrocervical trunk arises from the first part of the subclavian artery and gives rise to three branches. Costocervical Trunk the costocervical trunk arises from the back of the second part of the subclavian artery on the right side, but on the first part on the left side. Subscapular Artery (Inferior Scapular Artery) this artery is the largest branch of the axillary artery. It anastomoses with the lateral thoracic, intercostal arteries and deep branch of the transverse cervical artery, and supplies muscles of the chest wall. Deep Cervical Artery the deep cervical artery arises in most cases from the costocervical trunk but may be a branch of the subclavian artery. Branches Circumflex scapular artery Infrascapular artery Lateral border of the scapula (dorsal thoracic artery) Muscular branches Axillary Artery. Anterior Circumflex Humeral Artery this artery is a small branch that is located in front of the surgical neck of the humerus. It supplies the head of the humerus and shoulder joint and may have common origin with the posterior circumflex humeral artery. Branches Superior thoracic artery (highest) Thoracoacromial (acromiothoracic) artery Pectoral branch Acromial branch Clavicular branch Deltoid branch Lateral thoracic (lateral mammary branches) Subscapular artery Anterior circumflex humeral artery Posterior circumflex humeral artery Posterior Circumflex Humeral Artery. It arises from the third part of the axillary artery and winds around the surgical neck of the humerus and distributes branches to the shoulder joint, deltoid, teres major and minor, and long and lateral heads of triceps. The descending branch anastomoses with the deltoid branch of the arteria profunda brachii, the anterior circumflex humeral artery, and with the acromial branches of the suprascapular and thoracoacromial arteries. Superior Thoracic Artery (Highest Thoracic Artery or Arteria Thoracica Suprema) the superior thoracic artery is a small vessel and arises from the first part of the axillary artery. Alar Thoracic Artery (Variation) the subscapular, circumflex humeral, and profunda brachii arteries may arise as a common trunk. The axillary artery may divide into radial and ulnar arteries or give off the anterior interosseous artery of the forearm. The subscapular, the lateral thoracic, and pectoral arteries may be part of a common trunk. It begins at the lower border of the tendon of the teres major, ending 1 cm below the elbow, dividing into radial and ulnar arteries. It runs down the arm, medially to the humerus and gradually moving to the front of the bone.
© 2025 Adrive Pharma, All Rights Reserved..