General Information about Antivert
One of the main advantages of Antivert is its effectiveness in preventing motion sickness. The treatment is usually taken about an hour before traveling, and it could present aid for up to 24 hours. This makes it a convenient option for those who have lengthy journeys ahead of them. It can be used on a daily basis for people who experience constant motion illness, corresponding to sailors or pilots.
While Antivert is primarily used for motion illness, it may also be prescribed for different situations such as vertigo. Vertigo is a sensation of dizziness or spinning, usually related to inner ear problems. Antivert may help alleviate symptoms of vertigo by blocking the release of histamine within the inside ear, decreasing the stimulation of nerve cells that trigger dizziness.
In conclusion, Antivert is a reliable medication for the prevention and therapy of motion illness and vertigo. Its effectiveness, minimal unwanted side effects, and availability in various types make it a popular selection for many individuals. However, as with any treatment, it's crucial to use it as prescribed and observe the doctor’s directions to ensure its security and effectiveness. With Antivert, motion illness and vertigo can now not be a hindrance to your travels and day by day activities.
Antivert, also identified by its generic name meclizine, belongs to a group of medications known as antihistamines. It works by blocking the action of histamine, a chemical within the physique that is liable for inflicting signs of movement illness. Antivert is used for the prevention and therapy of nausea, vomiting, and dizziness related to movement illness.
Motion illness is a typical downside that impacts a giant number of individuals. It is characterised by emotions of dizziness, nausea and vomiting while traveling in a car, similar to a car, airplane, or boat. This could be a main inconvenience for those who enjoy touring or need to commute for work. Fortunately, there's a medication that may help alleviate these signs – Antivert.
Antivert is out there in varied varieties, together with tablets, chewable tablets, and oral suspension. The dosage and frequency of the treatment will depend on the individual’s age, weight, and severity of signs. It is essential to consult a physician earlier than taking Antivert, especially for folks with a history of medical situations or those who are taking other medicines. Pregnant and breastfeeding girls also wants to seek medical recommendation earlier than utilizing Antivert.
Another advantage of Antivert is that it has minimal side effects. Unlike different movement sickness medicines, Antivert does not cause drowsiness or sedation. This is a big advantage for those who need to stay alert whereas traveling, particularly when driving or operating heavy machinery. It can be safe to make use of for children above the age of 12, making it a great choice for household journeys.
A virtually infinite number of environmental experiences and gene × environment interactions intervene silicium hair treatment generic 25 mg antivert overnight delivery. The authors acknowledged that depression, traumatic stress, and cerebrovascular disease are three such factors. Admitting the infant stage of empirical data collection, admitting the likelihood that some aspect of these curves may later be proven inaccurate, this graphic display should raise eyebrows. Although Cushing (1917) [281] and, more explicitly, Osnato and Giliberti (1927) [146] proposed that concussion may precipitate neurodegeneration and in spite of clinical reports since that of Martland (1928) [282] that multiple concussions may cause permanent brain damage it is only since about 1990 that neurobiologists have escalated their attack on this question. Second, media attention to the problem of dementia pugilistica among those who earlier pursued contact sports has increased. The author tentatively proposed the possibility that traumatic encephalopathy with an apparently static and persistent course possibly exhibits somewhat different neurobiological features compared with traumatic encephalopathy with an apparently progressive course [284]. It remains to be seen whether any categorical pathophysiological difference justifies either distinction. Be that as it may, abundant evidence has emerged that experimental and clinical concussion are associated with changes in the expression of many potentially toxic proteins typically associated with neurodegenerative disease, including A42, hyperphosphorylated tau, and -synuclein. It is premature to evaluate the evidence of this and other possible late sequelae. Although the resulting picture will surely be revised, it seems to be a reasonable synthesis of the state of the art. Of course, viewing this landscape of internal melee, two questions immediately come to mind: One: what is the minimal perturbation of the brain that provokes this chain reaction Three later chapters in this brief text will attempt to sort that out in so far as the state of the art allows. And unless and until we can better guess the magnitude of that total impact, we cannot fairly judge whether the net effects of concussion are merely tragic or catastrophic. If so, do there exist modifiable factors for which intervention might 72 73 1: What is a Concussive Brain Injury Additive effects of traumatic brain injury and other risk factors on dementia incidence (A) Cumulative incidence of dementia. Is discovering an effective post-concussive intervention a priority for brain health of the order of magnitude of fighting a Zika epidemic Or, instead, of the order of magnitude of fighting maternal and infant undernutrition, cerebrovascular disease, or air pollution all suspected of massive and tragic influence on our planet-wide metrics Setting aside the growing suspicion that one or more concussions may either cause, or lower the threshold for, disabling neurodegeneration, what has empirical science suggested as the explanation for persistent or lifelong clinical distress in some concussed persons Perhaps even more interestingly, whether or not a patient is aware of brain dysfunction, whether or not a neuropsychologist can detect brain dysfunction, might brain dysfunction nonetheless persist Laboratory investigations can provide valuable hints, but rodents are shy about enumerating their subjective symptoms, and hard to engage in cognitive tasks during imaging. Despite the glint of gold in the recent imaging literature, however, two caveats perhaps deserve mention. It seems to participate in multiple processes, including myelination, osmolality regulation, and energy production. Some studies have reported increases after injury (perhaps reflecting lipid peroxidation and recovery); others have reported no change. If, on the other hand, brain injury changes Cr concentration (and especially if the direction of change is variable), then that ratio cannot be interpreted. It remains to be seen: (1) what absolute or relative levels of these three metabolites reflect what physiological changes; (2) whether the commonly reported ratios detect or predict lasting cerebral harm; and (3) to what degree individual variation (for instance, in the mechanism of concussion, the time after impact, or the demographics and genetics of the patient) complicates interpretation of those ratios. This provides further evidence that symptoms, signs, or neuropsychological test results do not accurately reflect brain health. This evidence supports the virtually universally acknowledged fact, empirically described since Koch and Filehne hammered luckless dogs in 1874 [97], that a second impact during the period of metabolic vulnerability causes a brain injury far more disabling than would otherwise be expected for a blow of that force. However, that reduced ratio was not confined to those with brain injury: reduced Cr/Cho was found in subjects who complained of post-concussive-type symptoms, whether or not they had had brain injuries. Again, the evidence is ineluctable that post-concussive complaints are associated with altered brain function. The only question is the degree to which causality is rightly attributed to the impact. Yet the jury is out on the validity of metabolites or metabolite ratios as markers of brain damage. Present methods do not measure neuronal activity, but merely infer it from changes in blood oxygenation. The normal "resting state," normal patterns of connectivity, or normal patterns of response to tasks have not been defined in ways that permit robustly reliable comparison across centers. External confirmation of validity for instance, clinico-imaging-pathological correlation showing that a given complex temporo-spatial pattern of relative hyper- and hypo-activations sensitively and specifically identifies a neurobiological change is just beginning. Numerous studies of concussed individuals in the "chronic" phase (setting aside, for a moment, the question of clinical "recovery") report patterns of hyper- and/ or hypo-activation persisting as long as 3. Nor was it surprising to learn that athletes who developed post-concussive depression still showed reduced activation in the dorsolateral prefrontal cortex and striatum on average six to seven months later [315] or that soldiers exposed to mild blast injuries exhibit abnormal cerebral function on average 964 days after the event [307]. As neuropsychologists devised increasingly sensitive tests, it became apparent that many concussed patients who look and feel neurologically fine are nonetheless somewhat cognitively inferior to their baselines [321]. What is one to say about a patient who has no complaints, a normal neurological examination, and no apparent neuropsychological impairment, when his neuroimaging reveals persistent alterations in processing Both resting studies and activation studies, in which the brain is scanned while performing a task, report similar conclusions.
Their comment introduces the fact that multiple features of occupational status predict worse outcome medications diabetic neuropathy discount 25 mg antivert free shipping. These include pre-morbid unemployment [797], low occupational category [425, 797, 800, 801], low occupational satisfaction, limited independence, and limited decision making at work [131, 678, 800]. A related finding was reported by Rutherford, 1977 [800]: "Post-concussion symptoms were more frequent in. It is not, however, a meaningful sign of brain health because not everyone likes working, and some people like their jobs more than others. Some have painful extracranial injuries and never receive accurate diagnosis or effective interventions for their ancillary disabilities. On the other hand, for many people work lends structure and meaning to life and self. Although sparse empirical research is available to buttress that argument, the present author cannot restrain expressing his personal conviction: far too few concussed persons receive the education, rehabilitation, occupational therapy consultation, work-hardening, emotional support, and frankly passionate exhortation from clinicians, family, and friends required to get them back on the horse. This question might seem rhetorical, or even circular, like, "why is a bad life associated with a bad life Race or ethnicity may or may not be stressful; some minority communities flourish. A final common cerebral pathway linking social life, pre-morbid brain health, and concussion outcome Social disadvantage potentially limits such reserve not only by all of the unequivocally damaging effects of stress but also perhaps by compromised capacity for adaptation in the face of cell loss or circuit disruption. Just as a better-educated middle-aged adult with a more cognitively challenging job tends to maintain his or her brain fitness longer in the face of neurodegeneration, so might socially advantaged people tend to have brains fitter to regenerate from the neurometabolic melee. But what does "brain reserve" mean in terms of tissue cells and organelles and molecules More agile incorporation of dentate gyrus pluripotential stem cells into functional hippocampal circuits He defers to the forthcoming generation of neuroscientists who will hopefully be dissatisfied with platitudes and push the envelope to find root physiological mediators. Even then, a unitary neurobiological process is both unlikely to explain the jeopardy of the underclass and unlikely to be amenable to post-injury treatment. Pending easing of inequality, many health outcomes will forever be worse among our disadvantaged. On the Drama of Attribution the defense attorney assumes his gravest visage: She is depressed because she expected a bad outcome. She is depressed because she imagines herself to be more depressed than she was before the accident. In the literature, the clinic, and the forensic setting, one still encounters prickly clashes between those who are wedded to one explanation for a symptom versus those who are wedded to another. So long as there is money or blame to be dispensed, there will be a drama of attribution. The drama of attribution is the affect-laden effort to assign proportional causality. Back in the 20th century a writer could always find peers who would permit publication of a claim that only 10% of concussed persons exhibit long-term dysfunction. Some writers could even publish claims that prolonged symptoms could not possibly be due to damaged brain tissue, and therefore must be due to imagination or fakery. This essay, this book, is just one of many recent resources offering a step up from that slough of anti-science. Hopefully, editors and reviewers and judges and juries will henceforth reject such egregious misrepresentations of the empirical facts. It is entirely possible that a large number of factors other than immediate tissue change due to abrupt external force are operative. Attribution is not, however, amenable to black-and-white answers along the lines of "organic" versus "psychological," "neurological" versus "functional," or "conscious" versus "unconscious. If the boastful pronouncement "It is because she was depressed before" were not silly enough, then "She is mostly depressed because she was depressed before but somewhat depressed because she is upset about her accident" is hysterical. What detracts from the humor is that clinicians sometimes say such things aloud as if medical knowledge was being invoked in good faith. Pending a remarkable advance in our ability to parse human distress, humility is the guiding byword. By way of illustration, please again consider Georgia, our injured 29-year-old teacher and equestrian enthusiast. As previously noted: can one really apportion causality to one or the other factor when the two are inextricably intertwined She missed days at work, stopped virtually all recreational and avocational activities, and put her marriage plans on hold. On interview it seemed that some of the environmental factors contributing to her on-again-off-again depression in the decade prior to trauma were ongoing such as an emotionally withdrawn father and critical mother and others were variable such as the attentiveness of her current boyfriend and her performance evaluations by the new school principal. Her parents provided superficial support after the injury, showing the flag a couple of times at the hospital. Discussing the impact of the concussion, she expressed what seemed to be somewhat excessive concerns that she would never ride again (bad expectations). At the same time, she seemed realistically aware, and hopeful, that her memory problems were improving. During her sadder clinical visits, she described her life before the injury and her life after the injury as night and day. This did not seem so much a good-old-days bias as a negative and pessimistic appraisal of her genuine progress toward recovery. Getting a lawyer at the behest of her parents did not seem to help or hurt; her self-reports followed the same uneven trajectory of slow improvement before and after she entered litigation until her deposition when she was exposed to a cruelly accusatory insurance attorney, after which her depression deepened. What neurologist on earth would venture to say: "Georgia exhibits a 13 percentile increase from her pre-morbid dysfunctionality.
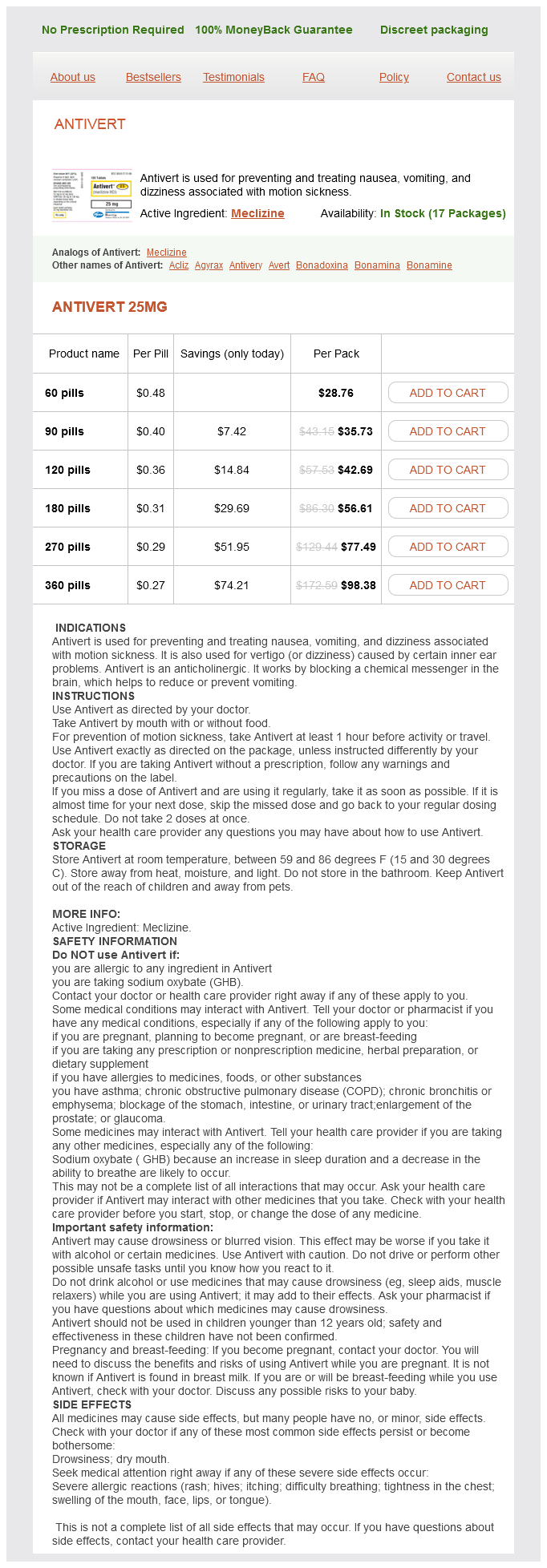
Antivert Dosage and Price
Antivert 25mg
- 60 pills - $28.76
- 90 pills - $35.73
- 120 pills - $42.69
- 180 pills - $56.61
- 270 pills - $77.49
- 360 pills - $98.38
For instance treatment plan for depression antivert 25 mg buy overnight delivery, evidence suggests that older patients tend to be happier to let the doctor decide for them, but the question remains whether that is because of aging effects or because of a cohort effect having been raised within a culture of deference to doctors [159]. Similarly, younger, more educated patients and women apparently want more input into decision making, but that seems to depend on the severity of the illness [160]. The second problem is the more serious: doctors are bad at figuring out what patients want [157]. So the most compassionate, liberal-minded physician may nonetheless have a devil of a time intuiting what model of care will be most helpful for the frightened stranger on the gurney. As Goske and Bulas put it: the theoretical risk from radiation-induced cancer is projected onto a background of a frequent disease (nonfatal cancer) in the general population with a life-time risk of almost 40% in both men and women. To further complicate the discussion, the risk of radiation-induced cancer is based on population risk, not risk to individual patients. Citing Hippocrates, Maimonides, the Declaration of Helsinki, and the American Medical Association Code of Medical Ethics, the author opines that radiologists "respect the rights of patients by providing comprehensive and unbiased information about the tests" ([166], p. He cites a Wisconsin Supreme Court decision: "The standard to which a physician is held is determined. But the problem with this approach is that it dismisses a theoretical risk without considering a real risk. The most common refers to discussing the theoretical risk of radiation-related cancer. The second and relatively neglected use is discussing the real risk of forgoing an examination. It is understood, of course, that emergency management involves special pressures and exceptions, and that some concussed persons cannot fully participate in decision making. How good is so-called informed consent at accomplishing its ostensible intended purpose A discussion of this subject would be incomplete if it assumes that the typical institutional review board-approved process has utility. Evidence exists that a majority of patients do not understand the procedures or the risks when they read and sign informed consent forms. Whether they understand the words or not, patients tend to be influenced by illogical biases [163]. Moreover, the needs and desires for information vary widely between patients [164]. The risk that needs discussion especially when physicians are itching to withhold the scan is missed lesions. Some may be confused into thinking that the question is what matters to them, what with all their knowledge, experience, and wisdom Most doctors, thankfully, wish to do the right thing, if only that were clarified. If your institution grants (or tolerates) physician discretion, you have two scientifically defensible, cost-efficient, and ethically virtuous options: 1. With regard to cost containment, it is undeniable that we must collectively reduce the use of tests. Different physicians, of course, will feel more or less compunction about taking the cost containment initiative into their own hands. An examination of the role that physicians play in the control of health care costs suggests that unilateral rationing decisions by individual physicians at the bedside are morally unacceptable. Such decisions are arbitrary, ineffective in distributing health care resources, and formally unjust. As Ladd [172] pointed out, "Although the standards of informed consent apply in emergency care, there seems to be discrepancies between theory and practice, and emergency physicians may be more guilty than others of unjustified paternalism" ([172, p. If a doctor is leaning toward ordering a cerebral angiogram, the risk of generating a permanent neurological complication (according to one meta-analysis [173]) is only 0. Emergency department discharge of patients with a negative cranial computed tomography scan after minimal head injury. Magnetic resonance imaging improves 3-month outcome prediction in mild traumatic brain injury. Traumatic brain injury in the United States: Emergency department vists, hospitalizations and deaths 20022006. Magnetic resonance imaging application in the area of mild and acute traumatic brain injury: Implications for diagnostic markers Abnormalities on magnetic resonance imaging seen acutely following mild traumatic brain injury: Correlation with neuropsychological tests and delayed recovery. Servadei F, Teasdale G, Merry G, Neurotraumatology Committee of the World Federation of Neurosurgical Societies. Defining acute mild head injury in adults: A proposal based on prognostic factors, diagnosis, and management. Clinical policy: Neuroimaging and decision making in adult mild traumatic brain injury in the acute setting. Scandinavian guidelines for initial management of minimal, mild, and moderate head injuries. Evaluation and management of mild traumatic brain injury: An Eastern Association for the Surgery of Trauma practice management guideline. Summary of evidence-based guideline update: Evaluation and management of concussion in sports: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Adult trauma clinical practice guideline: Initial management of closed head injury in adults, 2nd edition. Scandinavian guidelines for initial management of minimal, mild and moderate head injuries in adults: An evidence and consensus-based update. Reliability of clinical guidelines in the detection of patients at risk following mild head injury: Results of a prospective study.
© 2025 Adrive Pharma, All Rights Reserved..