General Information about Actos
Several scientific trials have been performed to gauge Actos's effectiveness in managing kind 2 diabetes. The studies have proven that Actos can significantly lower blood sugar levels, leading to improved glycemic control. Additionally, Actos has been found to have a constructive effect on different well being markers, including blood stress and levels of cholesterol.
In conclusion, Actos has proven to be a priceless treatment within the management of sort 2 diabetes. Its effectiveness in controlling blood glucose ranges and potential constructive impact on other well being markers has made it a well-liked selection among physicians. However, as with any medicine, it is crucial to debate any potential dangers and side effects along with your doctor. With proper monitoring and adherence to your healthcare provider's instructions, Actos may help improve the quality of life for individuals dwelling with sort 2 diabetes.
However, like all medication, Actos comes with its own set of potential side effects. The most typical unwanted facet effects embrace weight achieve, fluid retention, and an elevated risk of bone fractures. There have also been some considerations about Actos's potential hyperlink to an elevated danger of bladder cancer. While the proof is inconclusive, it's essential to debate any potential dangers together with your healthcare supplier.
Type 2 diabetes is a continual situation that impacts millions of individuals worldwide. It occurs when the body is unable to properly use insulin, a hormone that regulates blood sugar ranges. As a outcome, the blood sugar levels within the body turn out to be elevated, resulting in a wide range of well being problems such as heart illness, nerve damage, and kidney issues. In the previous few decades, there have been advancements within the therapy of kind 2 diabetes, and Actos (Pioglitazone) has emerged as a well-liked treatment for controlling high blood sugar.
Actos is often prescribed along with correct food plan and exercise to help handle blood sugar ranges. It can additionally be used in combination with different diabetes medicines, similar to metformin or insulin. However, it shouldn't be utilized in patients with sort 1 diabetes or diabetic ketoacidosis, a severe condition the place the body produces excessive ranges of acidic substances called ketones.
One of the main advantages of Actos is that it's taken orally, making it a handy option for patients who could have difficulty with injections. It can be obtainable in various strengths, permitting for individualized dosing based mostly on the affected person's wants. Actos is generally properly tolerated and has a low threat of inflicting low blood sugar levels, a typical aspect impact of some other diabetes medications.
People with a historical past of coronary heart disease or coronary heart failure may have an increased risk of cardiovascular unwanted aspect effects whereas taking Actos. It is crucial to tell your doctor of any pre-existing medical circumstances and medications you are taking to ensure Actos is protected for you to use.
Actos is an oral medication that belongs to a category of drugs generally identified as thiazolidinediones. It works by rising the physique's sensitivity to insulin, permitting it to use insulin more successfully. This leads to higher blood sugar control and reduces the chance of complications associated with high blood sugar ranges.
Morbidity remains elevated because of a greater likelihood of recurrent infective endocarditis diabetes mellitus retinopathy order actos 30 mg otc, heart failure, and embolism or, if a valve is replaced, the risk of anticoagulation, valve thrombosis, or additional valve surgery. The identification of infective endocarditis requires the integration of clinical, laboratory, and echocardiographic findings. Note: Cases are defined clinically as definite if they fulfill two major criteria, one major criterion plus three minor criteria, or five minor criteria; cases are defined as possible if they fulfill one major and one minor criterion or three minor criteria. Cases are rejected if there is a firm alternate diagnosis explaining evidence of infective endocarditis; resolution of infective endocarditis syndrome with antibiotic therapy for <4 days; no pathologic evidence of infective endocarditis at surgery or autopsy, with antibiotic therapy for <4 days; or criteria for possible infective endocarditis are not met, as above. Provide cost-effective antimicrobial therapy determined by the likely or identified pathogen, drug susceptibilities, hepatic and renal function, drug allergies, and anticipated drug toxicities 5. The team should include cardiologists, cardiac surgeons, and specialists in infectious disease. Class I recommendations are conditions for which there is evidence, general agreement, or both that a given procedure or treatment is useful and effective. Level of evidence is listed as A (data derived from multiple randomized clinical trials), B (data derived from a single randomized trial or nonrandomized studies), and C (consensus opinion of experts). Treatment usually is started in the hospital, but for select patients it is often completed in the outpatient setting so long as defervescence has occurred and follow-up blood cultures show no growth. An extended duration of therapy is required, even for susceptible pathogens, because microorganisms are enclosed within valvular vegetations and fibrin deposits. In addition, high bacterial concentrations within vegetations may result in an inoculum effect that further resists killing (see Chapter 24 for additional discussion). Many bacteria are not actively dividing, further limiting the rate of bacterial death. Tables 111-4 to 111-7 summarize these recommendations, which are discussed in more detail in the following sections. Tables 111-8 and 111-9 list drug dosing and monitoring recommendations for adult and pediatric patients. Because these guidelines focus on common causes of endocarditis, readers are referred to other references for more in-depth discussion of unusually encountered organisms. Viridans group streptococci refers to a large number of different species, such as Streptococcus sanguinis, Streptococcus oralis, Streptococcus salivarius, Streptococcus mutans, and Gemella morbillorum. Streptococcal endocarditis is usually subacute, and the response to medical treatment is very good. Streptococcus gallolyticus (formerly known as Streptococcus bovis) is not a viridans group streptococcus, but it is included in this treatment group because it is penicillin sensitive and requires the same treatment. Endocarditis caused by Streptococcus pneumoniae, Streptococcus pyogenes, and group B, C, and G streptococci are uncommon, and their treatment is not well defined. A tolerant organism is inhibited but not killed by an antibiotic normally considered bactericidal. Despite some animal studies of endocarditis suggesting that tolerant strains do not respond as readily to -lactam therapy as nontolerant ones, this phenomenon is primarily a laboratory finding with little clinical significance. Indications for surgery include heart failure, persistent bacteremia, persistent vegetation, an increase in vegetation size, or recurrent emboli despite prolonged antibiotic treatment, valve dysfunction, paravalvular extension (eg, abscess), or endocarditis caused by resistant organisms (eg, fungi or gram-negative bacteria). Additionally, studies evaluating postsurgical outcomes and associated mortality are limited such that a specific risk prediction system has not been established. The role of surgery in the management of infective endocarditis is increasing; however, the duration of antibiotic therapy post-surgery is unclear and can depend on whether prosthetic material was inserted and if resected tissue is culture positive or culture negative. Regimens indicate treatment for left-sided endocarditis or complicated right-sided endocarditis; uncomplicated right-sided endocarditis may be treated for shorter durations and is described in the text. If short term, 2 week therapy is desired, the guidelines suggest either high-dose parenteral penicillin G or ceftriaxone in combination with an aminoglycoside. Although streptomycin was listed in previous guidelines, gentamicin is the preferred aminoglycoside because serum drug concentrations are obtained easily, clinicians are more familiar with its use, and the few strains of streptococci resistant to the effects of streptomycin-penicillin remain susceptible to gentamicinpenicillin. The decision of which regimen to use depends on the perceived risk versus benefit. For example, a 2-week course of gentamicin in an elderly patient with renal impairment may be associated with ototoxicity, worsening renal function, or both. Furthermore, the 2-week regimen is not recommended for patients with known extracardiac infection. On the other hand, a 4-week course of penicillin alone generally entails greater expense, especially if the patient remains in the hospital. Monotherapy with once-daily ceftriaxone offers ease of administration, facilitates home healthcare treatment, and may be cost-effective. No cardiovascular risk factors such as heart failure, aortic insufficiency, or conduction abnormalities 3. Patients should be managed by a multidisciplinary team that includes specialists in cardiology, cardiovascular surgery, infectious diseases, and clinical pharmacy. Duration of therapy for culture-negative endocarditis may be variable and should be based on clinical course and recommendations from infectious diseases consult. Haemophilus parainfluenzae, Haemophilus aphrophilus, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, and Kingella kingae. Abiotrophia defectiva and Granulicatella species have nutritional deficiencies that hinder growth in routine culture media. Some authors question the need for combination therapy in relatively resistant streptococci, emphasizing that few human data suggest that patients with endocarditis caused by these organisms respond less well to penicillin alone.
However diabetic levels order 45 mg actos mastercard, these agents should be avoided in urinary tract bleeding because of the risk of thrombosis and obstruction. The proposed regimen should take into account these risk factors and the most appropriate individualized therapy should be provided. Identification of these disorders is important so that inappropriate treatment is not given. Also known as hemophilia C, this deficiency is particularly common in people of Ashkenazi Jewish descent. Bleeding usually does not occur spontaneously, but excessive bleeding may occur after trauma or surgery. Most other deficiencies are inherited as autosomal recessive disorders and are rare. Some patients with abnormal molecules, such as a dysfibrinogenemia, may have an increased tendency to develop thromboembolic disease. Heat treatment, which includes dry and wet heat, is one method of viral inactivation. Wet heat is applied while the concentrate is in suspension or in solution (pasteurization) and appears to be more effective than dry heat. Other methods of viral inactivation include chemical (solvent detergent) and affinity chromatography with monoclonal antibodies. Prions are not inactivated by either solvent detergent treatment or by heat, so there is a risk of transmission. However, allergic-type reactions (eg, fever, chills, skin rashes, nausea, and headaches) have been reported. An age-related homeostasis mechanism is essential for spontaneous amelioration of hemophilia B Leyden. Venous thromboembolism prophylaxis and treatment in cancer: A consensus statement of major guidelines panels and call to action. The multifactorial etiology of inhibitor development in hemophilia: Genetics and environment. Sequential combined bypassing therapy is safe and effective in the treatment of unresponsive bleeding in adults and children with haemophilia and inhibitors. Parallel use of by-passing agents in haemophilia with inhibitors: A critical review. Exciting progress is being made in the development of new strategies for treating these types of disorders. The development of new factor products with improved pharmacokinetic properties as well as the advances in gene therapy may soon redefine the therapeutic landscape for these patients and improve their overall experience. Intracranial hemorrhage in a female leading to the diagnosis of severe hemophilia A and Turner syndrome. The North American Immune Tolerance Registry: Contributions to the thirty-year experience with immune tolerance therapy. The principal results of the International Immune Tolerance Study: A randomized dose comparison. Optimizing management of immune tolerance induction in patients with severe haemophilia A and inhibitors: Towards evidence-based approaches. Up to date concepts about von Willebrand disease and the diagnose of this hemostatic disorder. Current management of patients with severe von Willebrand disease type 3: A 2012 update. The diagnosis and management of von Willebrand disease: A United Kingdom Haemophilia Centre Doctors Organization guideline approved by the British Committee for Standards in Haematology. Von Willebrand disease and other bleeding disorders in women: Consensus on diagnosis and management from an international expert panel. Pharmacokinetics and safety of a novel recombinant human von Willebrand factor manufactured with a plasma-free method: A prospective trial. Therefore, the transition from pediatric to adult medical care has become a focus to further improve survival and quality of life. Frequent hospitalizations can interrupt schooling and result in employment difficulties. Later in life, chronic organ damage and cognitive or emotional impairment can develop. Patients can have one defective gene (sickle cell trait) or two defective genes (sickle cell disease). Although sickle cell disease usually occurs in persons of African ancestry, other ethnic groups can be affected. Multiple mutation variants are responsible for differences in clinical manifestations. Usual clinical signs and symptoms include anemia, pain, splenomegaly, and pulmonary symptoms. Sickle cell disease is identified through routine newborn screening programs available in all 50 states. Hydroxyurea decreases the incidence of painful episodes, but patients treated with hydroxyurea should be carefully monitored. Screening with transcranial Doppler ultrasound to identify children at risk accompanied by chronic transfusion therapy programs can decrease the risk of overt and silent stroke in children with sickle cell disease. Analgesic options include opioids, nonsteroidal anti-inflammatory agents, and acetaminophen. The patient characteristics and the severity of the pain should determine the choice of agent and regimen. Patients with sickle cell disease should be followed regularly for healthcare maintenance issues and monitored for changes in organ function. Other areas where the sickle mutation can be found include the Arabian Peninsula, the Indian subcontinent, and the Mediterranean region.
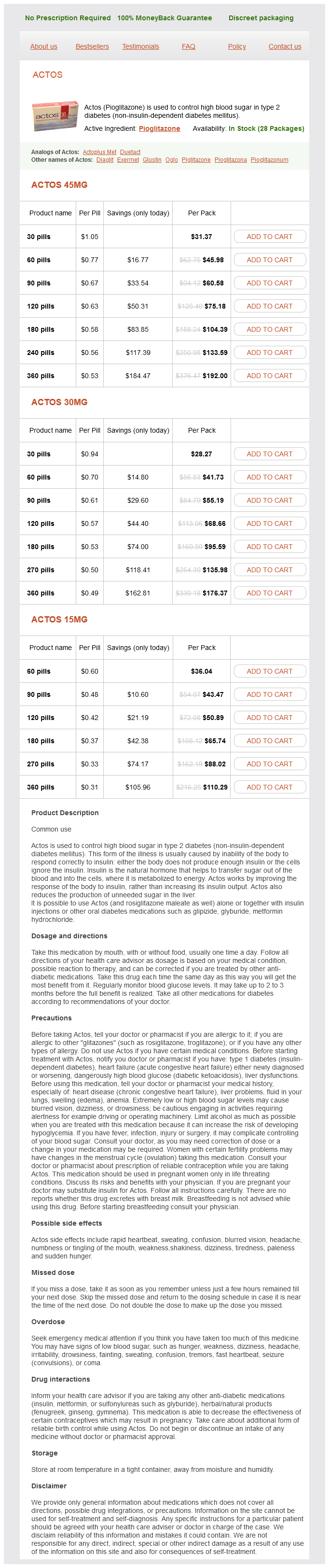
Actos Dosage and Price
Actos 45mg
- 30 pills - $31.37
- 60 pills - $45.98
- 90 pills - $60.58
- 120 pills - $75.18
- 180 pills - $104.39
- 240 pills - $133.59
- 360 pills - $192.00
Actos 30mg
- 30 pills - $28.27
- 60 pills - $41.73
- 90 pills - $55.19
- 120 pills - $68.66
- 180 pills - $95.59
- 270 pills - $135.98
- 360 pills - $176.37
Actos 15mg
- 60 pills - $36.04
- 90 pills - $43.47
- 120 pills - $50.89
- 180 pills - $65.74
- 270 pills - $88.02
- 360 pills - $110.29
If left untreated diabetes insipidus opposite buy generic actos pills, soft-tissue infection and osteomyelitis may occur, possibly requiring extensive debridement or amputation. Most dog bites are to the extremities,78 but the majority of bites to children less than 5 years of age are to the face and neck. However, infection may occur in up to 30% to 80% of serious cat bites, a rate more than double those seen with dog bites. Bites by others can occur to any part of the body, but most often involve the hands. Pasteurella multocida is part of the normal oral flora of up to 90% of cats; dog bites more commonly involve P. Pathophysiology the potential for infection from an animal bite is great owing to the pressure that can be exerted during the bite and the vast number of potential pathogens that make up the normal oral flora. Their teeth easily penetrate into bones and joints, resulting in a higher incidence of septic arthritis and osteomyelitis. A reduction in erythema, warmth, pain, and other signs and symptoms should be seen in 48 to 72 hours. Effective treatment of bite wounds includes avoidance of unnecessary antimicrobials that contribute to increased resistance, and minimizing toxicities and cost of therapy. Management of Bite Wounds 9 Bite wounds should be irrigated thoroughly with a copious volume of sterile water or saline, and the wound washed vigorously with soap or povidoneiodine in order to reduce the bacterial count in the wound. Clinical failures due to edema have occurred despite appropriate antibiotic therapy. In the case of animal bites, an immunization history of the animal should be obtained. Specifically, prophylaxis is more strongly recommended in patients with the following factors associated with increased risk for infection: immunocompromised; asplenic; advanced liver disease; preexisting or resultant edema of the affected area; moderate to severe bite-related injuries, especially to the hands or face; or bite injuries that have penetrated the periosteum or joint capsule. Amoxicillinclavulanic acid is most commonly recommended for oral outpatient therapy due to excellent activity against all likely pathogens, including Pasteurella and Eikenella. Failure to provide adequate initial treatment of bite wounds results in treatment failures and increased need for hospitalization for parenteral antibiotics. The length of antimicrobial therapy depends on the severity of the injury/infection. Most patients with clenched-fist injuries present for medical care after infection is already established. Wounds often have a purulent discharge, and decreased range of motion may be present. Wounds seen <8 hours or more than 24 hours after injury that show no signs of infection may not need to be cultured. White blood counts should be monitored for resolution of infection if initially elevated. Signs · Erythema, swelling, and clear or purulent discharge at site of infected wound. Animal bites: Other Diagnostic Tests · Radiographic evaluation should be performed if damage to a bone or joint is suspected. Because the rabies virus can be transmitted via saliva, rabies may be a potential complication of a bite. When the symptoms of rabies develop after a bite, the prognosis for survival is poor. Roughly 3% of rabies cases documented in animals were in dogs (the most frequent vectors are skunks, raccoons, and bats). If the animal is healthy and able to be observed for a 10-day period, active prophylaxis is only required if the dog develops signs of rabies. Aggressive antimicrobial use must be balanced against unnecessary administration of drugs that may lead to increased antimicrobial resistance, adverse effects, and cost. Evaluation of Therapeutic Outcomes Evaluation of treatment for either animal or human bites should follow the same general guidelines. Bite victims treated on an outpatient basis with oral antimicrobials should be followed up within 24 hours by either phone or office visit. For hospitalized patients with no improvement in signs and symptoms following 24 hours of appropriate therapy, surgical debridement may be needed. Physical therapy may be needed to improve complications such as residual joint stiffness and loss of function, particularly after human bites involving clenched-fist injuries. Incidence, microbiology, and patient characteristics of skin and soft-tissue infections in a U. Incidence and cost of hospitalizations associated with Staphylococcus aureus skin and soft infections in the United States from 2001 through 2009. Emergency department visit rates for abscess versus other skin infections during the emergence of community-associated methicillin-resistant Staphylococcus aureus, 1997-2007. Skin and soft tissue infections caused by community-acquired methicillin-resistant Staphylococcus aureus. Practice guidelines for the diagnosis and management of skin and soft-tissue infections: 2014 update by the Infectious Diseases Society of America. Skin and soft tissue infections caused by methicillinresistant Staphylococcus aureus. Community-acquired methicillinresistant Staphylococcus aureus skin and soft-tissue infections: management and prevention. Community-acquired methicillin-resistant Staphylococcus aureus: Epidemiology and clinical consequences of an emerging epidemic. Community-associated methicillin-resistant Staphylococcus aureus: Trends in case and isolate characteristics from six years of prospective surveillance.
© 2025 Adrive Pharma, All Rights Reserved..