General Information about Abana
Abana is also identified to have anti-inflammatory properties, which can be beneficial in reducing the risk of heart disease. Chronic irritation has been linked to numerous cardiovascular circumstances, and by decreasing inflammation, Abana may help to guard the guts and blood vessels from harm.
Another essential ingredient in Abana is Arjuna, a tree native to India. Its bark is rich in coenzyme Q10, which helps to improve coronary heart function and cut back cholesterol levels. Arjuna additionally accommodates antioxidants that defend the arteries from injury by free radicals and promote their elasticity, which is crucial for maintaining a wholesome blood move.
According to numerous studies, Abana has shown promising results in reducing levels of cholesterol and bettering coronary heart well being. In one research, participants taking Abana noticed a significant decrease in whole cholesterol levels and a 24% lower in LDL cholesterol after eight weeks of use. They additionally showed enhancements in their overall lipid profile and skilled no adverse effects.
In conclusion, Abana is an effective and pure treatment for managing levels of cholesterol and selling coronary heart well being. Its unique blend of herbs provides a holistic method to lowering cholesterol levels and protecting the guts from damage. With its confirmed monitor document and minimal unwanted effects, Abana is a protected and dependable choice for those seeking to maintain healthy levels of cholesterol. However, as with every medicine, you will want to consult with a healthcare skilled before starting any new supplement or treatment.
One of the vital thing elements in Abana is Guggulu, a resin extracted from the Indian myrrh tree. It has been utilized in Ayurveda for hundreds of years to treat numerous ailments, including high ldl cholesterol. Guggulu works by inhibiting the production of cholesterol in the liver and rising its breakdown. This helps to reduce the whole ldl cholesterol and low-density lipoprotein (LDL) or 'dangerous' levels of cholesterol in the blood.
The security profile of Abana is another benefit, as it does not cause any of the unwanted facet effects generally associated with traditional cholesterol-lowering drugs like statins. This is as a result of it's created from natural elements and is free from dangerous chemical compounds and synthetic components.
Cholesterol is a waxy substance that's present in every cell of the body. It plays an important position in various bodily capabilities, such as hormone manufacturing and digestion. However, excessive levels of cholesterol in the blood can increase the chance of coronary heart disease and stroke. This is the place medications like Abana are available – a pure and effective way to cut back cholesterol levels and enhance total well being.
Other herbs like Yashtimadhu (Licorice) and Shatavari (Asparagus) additionally play important roles in Abana's cholesterol-lowering properties. Yashtimadhu helps to decrease the absorption of cholesterol from the intestines and supports healthy liver function. Shatavari accommodates saponins, which help to scale back LDL ldl cholesterol and triglyceride levels. These and different ingredients in Abana work together to supply a comprehensive approach to managing levels of cholesterol.
Abana is an natural product developed by the Himalaya Drug Company, a leading world manufacturer of natural healthcare products. It is a combination of various herbs which have been historically used in Ayurvedic medication to maintain coronary heart well being and assist wholesome levels of cholesterol and triglycerides in the blood. The elements in Abana work synergistically to promote cardiovascular wellness and lower serum lipids.
Nucleolar damage correlates with neurotoxicity induced by different platinum drugs cholesterol levels example order line abana. Neuronal involvement in cisplatin neuropathy: Prospective clinical and neurophysiological studies. Histology and platinum content of sensory ganglia and sural nerves in patients treated with cisplatin and carboplatin: An autopsy study. Incidence of atypical acute nerve hyperexcitability symptoms in oxaliplatin-treated patients with colorectal cancer. Studies of peripheral sensory nerves in paclitaxel-induced painful peripheral neuropathy: Evidence for mitochondrial dysfunction. Taxane-induced peripheral neuropathy has good long-term prognosis: A 1- to 13-year evaluation. Toxicity profile of the immunomodulatory thalidomide analogue, lenalidomide: Phase I clinical trial of three dosing schedules in patients with solid malignancies. Lenalidomide plus dexamethasone versus thalidomide plus dexamethasone in newly diagnosed multiple myeloma: A comparative analysis of 411 patients. Single-agent bortezomib in previously untreated multiple myeloma: Efficacy, characterization of peripheral neuropathy, and molecular correlations with response and neuropathy. Bortezomib-associated peripheral neuropathy requiring medical treatment is decreased by administering the medication by subcutaneous injection in Korean multiple myeloma patients. Peripheral neuropathy experience in patients with relapsed and/or refractory multiple myeloma treated with carfilzomib. Treatmentrelated peripheral neuropathy in multiple myeloma: the challenge continues. Effects of eribulin, vincristine, paclitaxel and ixabepilone on fast axonal transport and kinesin-1 driven microtubule gliding: Implications for chemotherapy-induced peripheral neuropathy. The radiation-induced fibroatrophic process: Therapeutic perspective via the antioxidant pathway. Chronic arsenic toxicity in Bangladesh and West Bengal, India-a review and commentary. Neuropathy in arsenic toxicity from groundwater arsenic contamination in West Bengal, India. Organophosphates induce distal axonal damage, but not brain oedema, by inactivating neuropathy target esterase. Electrophysiological follow-up of patients with chronic peripheral neuropathy induced by occupational intoxication with n-hexane. Mechanisms of toxic injury in the peripheral nervous system: Neuropathologic considerations. Neurologic degeneration associated with nitrous oxide anesthesia in patients with vitamin B12 deficiency. Alcoholic neuropathy is clinicopathologically distinct from thiamine-deficiency neuropathy. Peripheral nerve functions in chronic alcoholic patients on disulfiram: A six month follow up. Revisiting the evidence for neuropathy caused by pyridoxine deficiency and excess. Dose response, coasting, and differential fiber vulnerability in human toxic neuropathy: A prospective study of pyridoxine neurotoxicity. Technology advances indicate neuronal energy balance and mitochondrial biogenesis, and fission and fusion are additional potential mechanisms. Diabetic polyneuropathy is the most common debilitating complication of diabetes, characterized by distal-to-proximal degeneration of peripheral nerve fibers and an ultimate loss of neuronal function. Two comprehensive reviews13,14 thoroughly describe the role of the glyoxalase system in the microvascular complications of diabetes and aging. The localization of Glo1 protein to small peptidergic sensory neurons was consistent across mouse strains, but the response to diabetes induction was not. Taken together, these data indicate a direct role of reactive dicarbonyls in neuronal damage and emphasize the importance of the enzyme systems responsible for their detoxification. Diabetes decreased expression of mitochondrial proteins and respiratory chain activity; however, an increase in superoxide was not detected. The effect of nutrient overload on the mitochondrial proteome and other intracellular energy sensing systems was thoroughly reviewed by Chowdhury. Differences between the two types of diabetes include levels of circulating insulin and insulin insensitivity, inflammation,4 and oxidized lipids. This occurs following heat shock or other cellular stressors and is met with the heat shock response, an increase in chaperone expression. In contrast to Schwann cells, sensory neurons are much more susceptible to hyperglycemia as indicated by the number of studies documenting cellular death and/or damage, decreased neurite outgrowth, slowing of nerve conduction and fiber loss. The effects of hyperglycemia on the mitochondrial proteome in primary sensory neurons were examined by Zhang,28 Urban,25,26 and Akude. Mitochondrial protein expression was significantly decreased and levels of superoxide were increased. Importantly, these were not prevention but intervention studies in two different strains of mice. The incretin family of peptides is a group of gut hormones, secreted in response to feeding, that enhance insulin secretion.
Protein zero (P0)-deficient mice show myelin degeneration in peripheral nerves characteristic of inherited human neuropathies cholesterol chart level discount 60 pills abana with visa. Neurological dysfunction and axonal degeneration in Charcot-Marie-Tooth disease type 1A. Myelin-associated glycoprotein is a myelin signal that modulates the caliber of myelinated axons. Mice lacking complex gangliosides develop Wallerian degeneration and myelination defects. Two diverent types of nerve pathology in patients with different P0 mutations in Charcot-Marie-Tooth disease. Electron microscopy of teased nerve fibers: Method permitting examination of repeating sructures of same fiber. As part of this primary directive, it has learned to separate "self " from "non-self," in order to limit autoreactive injury to healthy tissues, a process known as immunological tolerance. In autoimmune neuropathies, overriding tolerance to generate aberrant responses to self-antigens results in the development of immune-mediated injury to many different components of nerve. With respect to adaptive immune activation, both T cellmediated and B cell-mediated (humoral) pathways play key roles in pathogenesis, and thus the clinical manifestation of these conditions. Cytokines and other soluble molecules facilitate the inflammatory response, leading to demyelination, axonal injury, and breakdown of the bloodnerve barrier. Macrophages are particularly involved in phagocytosis of the myelin sheath, giving rise to segmental demyelination, a pathological and electrophysiological hallmark of many of these inflammatory neuropathy conditions. In particular the neuroimmunology of antiganglioside antibodies has been well defined experimentally, and is also helpful in phenotypic characterization of the disease subtypes. The underlying concept is that structurally homologous epitopes exist between invading pathogens and self-antigens that, when presented to the immune system in a way that overcomes tolerance, can inadvertently trigger an autoimmune response. Most notably, on binding to their ganglioside ligands that are expressed in nerve plasma membrane, they activate the complement cascade, thereby triggering a myriad of inflammatory consequences. Complement factors are plasma proteins that act to aid phagocytosis of pathogens via opsoninisation. After the cascade is triggered, inflammatory peptides such as C3b join the inflammatory cascade, with C3a being a catalyst in the formation of the pore-forming membrane attack complex (C5b-9), which then allows an aberrant influx of water and calcium into the intracellular environment of glial cells and axons, initiating injurious cascades and culminating in the characteristic nerve damage. Although weakness and sensory disturbance are classic features of all conditions, the onset, evolution, and symmetry of symptoms can help point toward a clinical syndrome. As mentioned previously, the trigger is typically a minor infection, Campylobacter jejuni, Mycoplasm pneumoniae, and a range of herpes viruses13 being typical causes. Diagnostic criteria include rapidly ascending paresis reaching its nadir within 4 weeks, areflexia, and sensory symptoms including pain. A product of plasma cell dyscrasia, it gives rise to a chronic, predominantly motor polyneuropathy. Clinically, this manifests as a chronic neuropathy with marked ataxia, though limb strength is relatively preserved. The archetypal phenotype in this group is a subacute sensory neuronopathy, which is defined as "subacute onset with a Rankin score of at least 3 before 12 weeks of evolution, onset of numbness, and often pain, marked asymmetry of symptoms at onset, involvement of the arms, proprioceptive loss in the areas affected. These typically manifest with asymmetrical sensorimotor features, with pain a predominant feature, though the underlying pathology can influence phenotype. However, there are many useful tests that can help define specific syndrome and help differentiate between conditions. Focusing on tests that specifically pertain to immune-mediated neuropathy, the clinical presentation can act as a guide to which tests to perform. The findings in vasculitic neuropathies are dependent on the underlying pathology. The most common feature, indicative of inflammation in intraspinal nerve roots, would be total protein elevation (>0. The most common nerve targeted for such a procedure is the sural nerve, a sensory nerve consisting of branches of the common tibial and common femoral nerves. Meaningful results are dependent on the sural nerve being affected by the pathology, and the preparation of the sample at pathological examination. Wallerian degeneration is a classic feature, often seen in neuropathies with vasculitic origins. This process has been documented in neuropathies associated with monoclonal gammopathies as well as in idiopathic, metabolic, and nutritional neuropathies. The pathology of immune-mediated neuropathies can map onto well-characterized clinical syndromes with their own pathological hallmarks. Demyelination hallmarks include conduction block, temporal dispersion, slowed conduction velocities, and prolonged F-wave latencies. Plasma exchange was initially the treatment of choice, with trials comparing best supportive care showing improvements in mobility and requirement for artificial ventilation. A marker of neuromuscular respiratory function is forced vital capacity, which should be monitored frequently and dictates consideration of artificial ventilation. Immobility also puts patients at risk of thromboembolism, and thus compression stockings and low molecular weight heparin are invariably used. Therapies include high-dose chemotherapy and stem cell transplant, alkylating agents such as melphanan, or targeted radiotherapy. The approach to systemic disease is long-term corticosteroids, with an additional agent such as cyclosporine. For aggressive neuropathies the addition of azathioprine, methotrexate, or other agents is suggested.
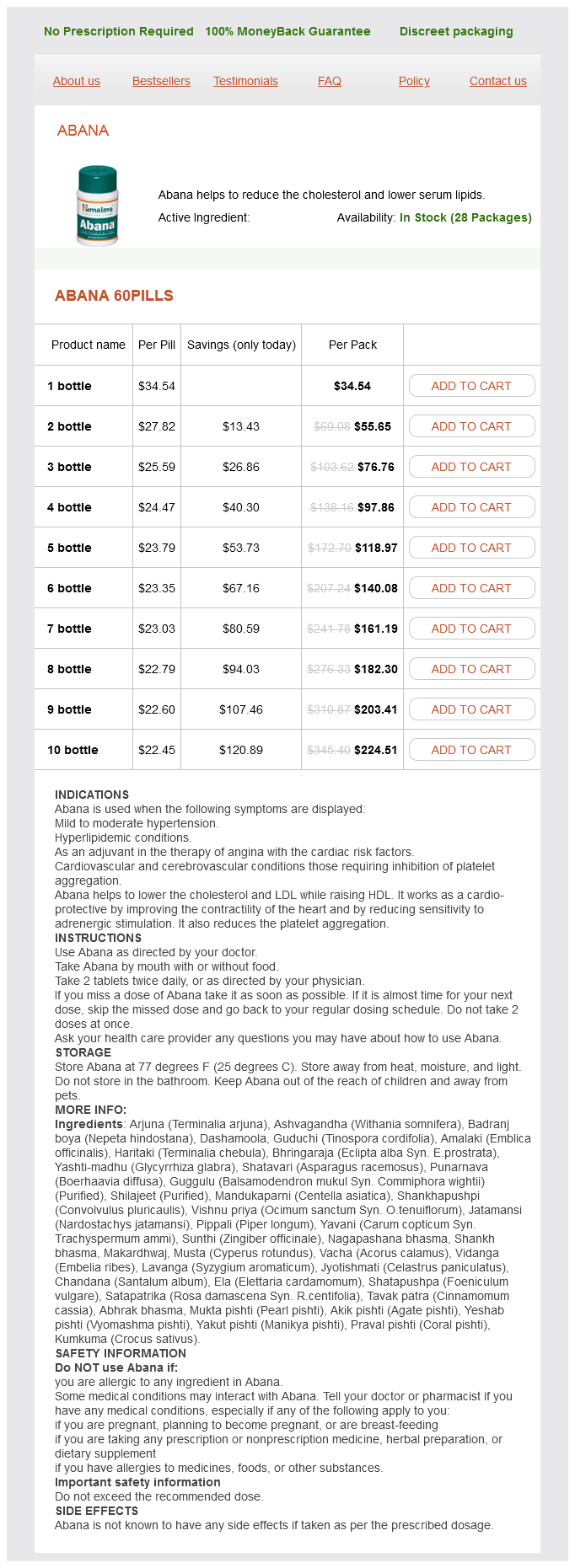
Abana Dosage and Price
Abana 60pills
- 1 bottle - $34.54
- 2 bottle - $55.65
- 3 bottle - $76.76
- 4 bottle - $97.86
- 5 bottle - $118.97
- 6 bottle - $140.08
- 7 bottle - $161.19
- 8 bottle - $182.30
- 9 bottle - $203.41
- 10 bottle - $224.51
Locomotor hyperactivity induced by blockade of prefrontal cortical alpha2-adrenoceptors in monkeys cholesterol medication elderly cheap 60 pills abana free shipping. Animal models concerning the role of dopamine in attention-deficit hyperactivity disorder. Depressed dopamine activity in caudate and preliminary evidence of limbic involvement in adults with attention-deficit/hyperactivity disorder. The roles of dopamine and noradrenaline in the pathophysiology and treatment of attention-deficit/hyperactivity disorder. Case-control genome-wide association study of attention-deficit/ hyperactivity disorder. Exome sequencing and unrelated findings in the context of complex disease research: ethical and clinical implications. Mitochondria are responsible for producing the energy for almost all cellular processes in nearly all the cells in the body. Paternally inherited mitochondria are typically destroyed during fertilization and persistence of paternally inherited mitochondria is often a cause or indicator of disease. When oocytes divide, mitochondrial chromosomes are distributed randomly leading to different percentages of heteroplasmy in different oocytes and eventually in the offspring. Primary mitochondrial diseases are among the most common inborn errors of metabolism. Presentations are very variable, as different individuals and different tissues within the same individual can have different levels of heteroplasmy. Because of the clinical variability, determining when to investigate for mitochondrial disorders is an active area of investigation. A number of sets of criteria have been developed to diagnose mitochondrial disorders. Although primary mitochondrial diseases can present with nearly any symptoms, common symptoms by organ system are listed in Table 61. Because the presentations are so variable and often associated symptoms are nonspecific, many investigators have worked to formulate "red flags," or signs or symptoms when clinicians should be increasingly suspicious for a primary disorder of mitochondrial energy metabolism. The majority of patients who are diagnosed with a primary mitochondrial disorder have heterogeneous presentations as mentioned. There are, however, a number of known syndromes caused by primary mitochondrial dysfunction of which the clinician should be aware. Leigh syndrome, otherwise known as "subacute necrotizing encephalomyopathy," was initially described in 1951. It is a progressive disease that can present at any age but most often in childhood. These patients also commonly experience cardiomyopathy, hearing and vision loss, peripheral neuropathy, ataxia, and lipomas. These patients commonly have normal development followed by progressive developmental disabilities, muscle weakness and fatigability, seizures, recurrent headaches and vomiting, and recurrent strokelike episodes (temporary hemiparesis, vision loss, etc. Additionally, patients with extremely similar phenotypes can have different genes mutated or complexes deficient. Neuroimaging can also provide crucial clues to the diagnosis of primary mitochondrial disorders. Some of these neuroimaging findings are seen in the specific syndromes mentioned, but there are other less pathognomonic findings seen commonly in these disorders. Elevation of lactate and the related reduction in N-acetylaspartic acid (particularly as compared to creatine) in many areas in the brain is nonspecific but in the correct clinical context can be strong evidence for underlying mitochondrial dysfunction. However, many clinicians were hesitant to perform such testing because it was invasive, had a high false negative rate, and could not always differentiate primary from secondary mitochondrial disorder. When performing tissue biopsy for mitochondrial disease diagnosis, a clinician first must decide what tissue to sample. The tissue with the highest yield is going to be the tissue most affected by the disease in the patient. The most commonly tested tissues are skin, skeletal muscle, liver, and cardiac muscle. Thus tissue should also be sent for biochemical analysis-spectrophotometric assays of respiratory chain enzyme activity and functional studies of intact mitochondria. Spectrophotometric assays assess the function of the respiratory chain complexes individually and in specific combinations. The activity levels are measured relative to a control enzyme (often citrate synthase). First, there is great interlab variability in these tests and so not all results are universally reproducible. Second, the activity levels are measured in vitro not in vivo and so the results may differ from the true function of that enzyme complex in the cytosolic cellular environment. Commonly ordered tests such as blood lactate and pyruvate can have false negatives and false positives. However, there are a number of tests that, when abnormal, especially in conjunction with other abnormalities, can signify that something is awry with mitochondrial energy metabolism. The synthesis of clinical, biochemical laboratory, genetic, and pathology data then leads the clinician to determine whether a primary disorder of mitochondrial metabolism is the correct diagnosis. Elevation in glycine, proline, sarcosine or tyrosine Low total free carnitine or low acyl:free carnitine ratio.
© 2025 Adrive Pharma, All Rights Reserved..